Alexander Tin's notes
tinalexander.github.io / notes / 2023 / 09 /
Learn more about this site and how to get in touch.
September 29, 2023
CDC officials on changes to pan-respiratory data website
- Source: webcast of Health Data Innovation Summit by CDC Foundation
- Date: broadcasted September 28, 2023
Matthew Ritchey, CDC [00:26:10]
So what we’re working is, right now, leveraging our DCIPHER and our PROTECT platforms as our main common operating platform.
And what this does is helps us integrate the data from multiple programs, knowing that we have things coming in, like in the hospital side, things that are naturally coming in from our NCIRD programs and various other places, all bring it together and synchronizing it in one place so that we can make it available for consistent use. So that’s a big effort that’s underway right now, and being leveraged specifically for the RVR work.
In that too, we also have a system called CDC Ready, which retrieves the data from DCIPHER and the PROTECT platforms and provides, again, that last mile delivery to our web content management system, to data.cdc.gov, to really help advance our efforts in being fully data transparent and then provides other outputs needed for reporting visualization and dissemination.
So again, it’s leveraging that common operating platform to help inform the overall common operating picture on the data visualization tools, kind of place in products. Again, it’s this idea about what does that common operating picture look like for this response.
That we’re really trying to take it and scale it and make sure it’s available in an enduring way for other future responses, as well as future respiratory seasons, knowing that this is not going to be the only respiratory season, it is an annual thing.
…
Matthew Ritchey, CDC [00:32:11]
We’re capitalizing on a model that was kind of started to really kind of gain a lot of steam during the COVID response was this idea.
We had a COVID update, so a product that we would use from our common operating picture and populate, and then send it out to our USG partners, kind of what is the current situational awareness around COVID, we’re repurposing that model, expanding it now for multiple respiratory diseases, as far as in this pan respiratory model and having this weekly respiratory virus update again, leveraging all the data, the same systems, that modular data products that we’re using for other purposes, but then specifically packaged for our USG partners.
And then finally, as this idea, that’s integrated offering at the bottom, and this is our website and what we’re working towards launching, we’ve already made some gains here early in September. We’re working to make further enhancements to this web offering.
So again, trying to create that kind of vertical stack, but also the horizontal wrapper, to bring a lot of the important information specifically for respiratory viruses together in one place.
…
Matthew Ritchey, CDC [00:33:08]
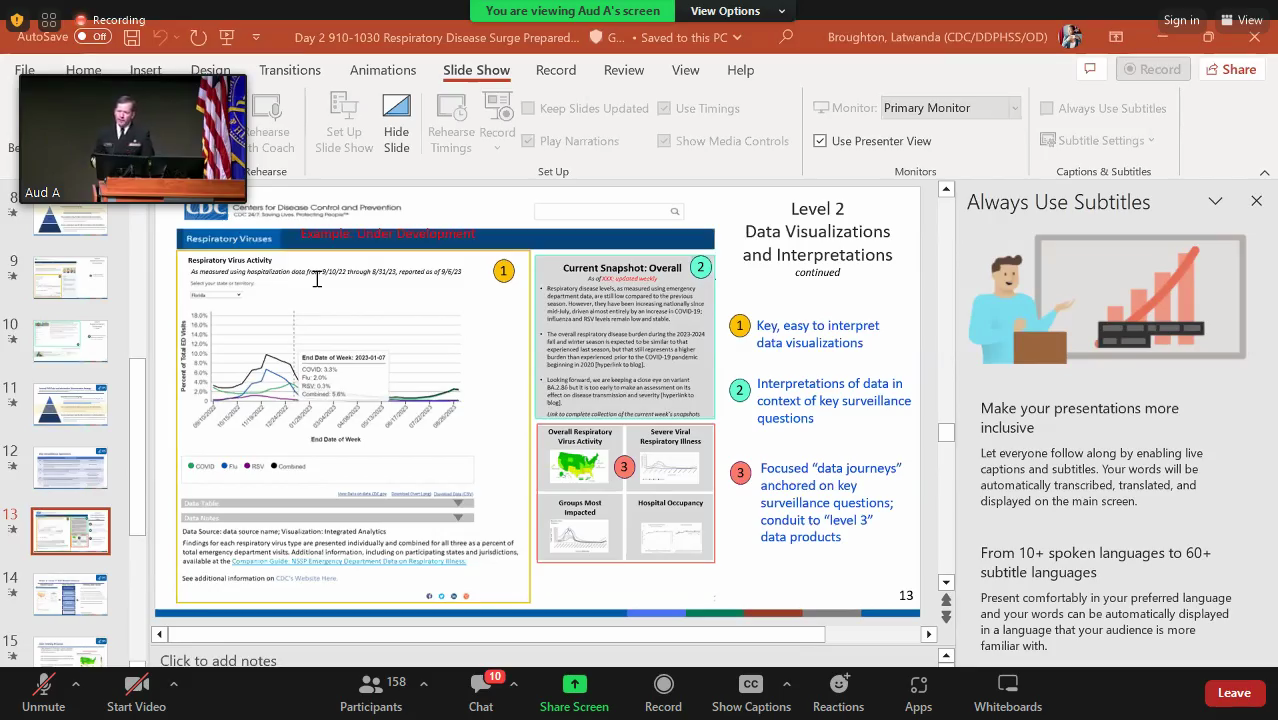
So walking through that strategy, just to kind of give you an idea of where we’re trying to move here is this kind of three level approach or three level strategy, level one, two and three.
So for level one, for respiratory viruses in particular, this is its initial landing page. We did a soft launch of this early in September on the sixth. And the idea that this is more of a communications tool. Again, if you think of that, that vertical stack, it’s that top part, that entry level for someone to come into our website or whatnot and say, ‘I want a little bit of data tell me like the most important thing, but then link it to some other guidance, tools, prevention, things of that nature.
So that’s what was launched on the sixth, the first iteration of that, we’re going to be continuing to iterate on that to make it more and more meaningful to the public as they kind of had that initial interface with our website around respiratory viruses.
…
Matthew Ritchey, CDC [00:33:51]
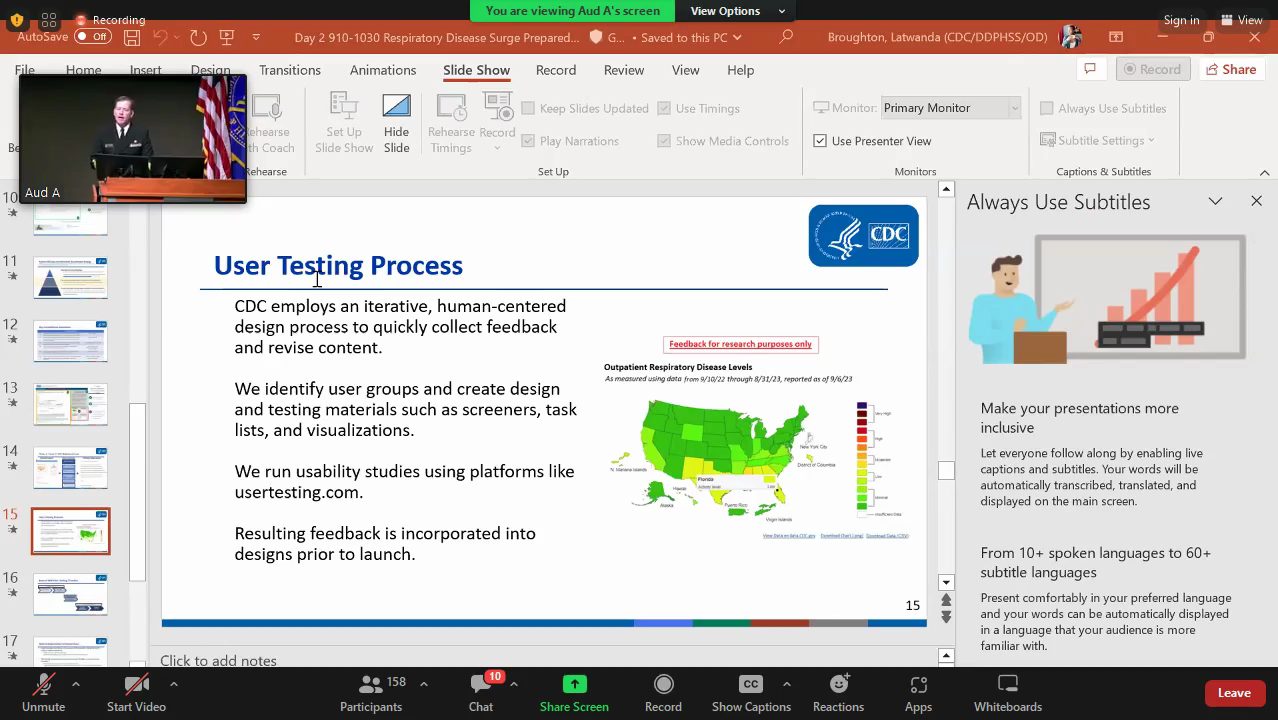
Next is what I really want to focus on today is that level two. And what level two is that wrapper. Knowing that we have a lot of really important things at our agency around pan-respiratory, but we also know there’s an opportunity there to sync up some of that information, put the three different conditions in context of each other, so the end user can say, ‘okay, overall, what does respiratory virus activity look like in the country? What does severity look like? Who is most impacted overall?’
And then if they wanna continue to go on create that wrapper into the level three, and the level three are all those other products that are already on our website, the COVID data trackers, a lot of the great flu products, some of the RSV products, how do we then create those linkages into those to makes again for a coherent journey for the end user?
…
Matthew Ritchey, CDC [00:34:36]
So for level one, again, this is what was launched the beginning of this month on September 9th. Again, it’s a little bit of a data snapshot right now. We’re leveraging our emergency department data, looking at trends for the three different conditions individually combined, so it kind of gives you a quick snapshot on, ‘Hey, are we– which direction are we going? What’s the overall burden?’
Again, we’re looking to continue to improve how this interface looks, but then again, also in that level, one space is this idea of linking the data then to action. And these are some of the, you know, understanding, okay, who is, what is my risk factor profile, or do I have people around me, my loved ones, that have coexisting medical conditions and things like that. And then how do we tie guidance to those collectively for respiratory disease at large, knowing that there’s some specific guidance that are tied to the specific conditions for COVID, influenza, RSV. So that’s level one.
For level two, is this idea about again, pulling it all together? Okay. What does respiratory disease look like overall from a data perspective?
So in that way that we’re trying to do this are more data stories, right? It’s not dashboards, but data stories. So you’d have a story, you have to kind of have like, what’s the hook, right? And the hook in these data stories are the surveillance questions, the key surveillance questions, some of the ones that we’re working on answering right now are, how bad is it? Where is it bad? Is it getting worse? And why? Are we seeing more severe disease? And if so, what’s driving that? Who’s at most at risk and how much burden is pleading placed on hospitals?
So those are some of the surveillance questions that we’re addressing right now.
…
Matthew Ritchey, CDC [00:36:04]
So again, in that kind of the layout of what the website’s going to be looking like as we go to launch here hopefully soon, is that we have a kind of a key visualization. This is one that you already saw, but up in the upper left hand side where people can kind of quickly discern kind of what’s the main take home. We have then that interpretation layer in the upper right hand side to say, ‘okay, what should you know about these data or other data that are pertinent to this overall story?’
And then finally we have these idea of data journeys in the bottom right hand corner, the number three here. And I’m gonna walk through a couple of those right now.
So in this first phase of our release, around the RVR data, in the data journey space, kind of in the center part of this, we want to focus on kind of what are the respiratory activity levels, what does severity look like, who are the groups most impacted and then hospital occupancy.
We’re also exploring other journeys as we kind of roll this out, knowing that we know this is gonna be iterative in nature. So things like vaccine data, things of that nature.
And then what we’ve done is mapped a lot of those primary data assets that Adi kind of mentioned in that first slide to these different data journeys, to these surveillance questions so that we can effectively package them and tell that story to the American public.
…
Ian Williams, CDC [00:52:53]
So the system that Dr Ritchey described to you here is really building on lessons that we learned, hard lessons that we learned both in COVID and then in subsequent responses like mpox.
I’m really trying to build the next generation of what a common operational picture, focusing on situational awareness data will look like.
And to really take a couple of steps back here, thinking about this common operational picture during public health emergencies at large, is to really bring together sort of in near real time from across the entire public health information, the data you need to make decisions.
This is information on tests, cases, testing, emergency room visits, healthcare system capacity, things like hospital admissions, ICU admissions, bed availability, mortality, other essential information like vaccine availability, administration of vaccines, or other therapeutics and diagnostic testing, having that essentially in one place in real time, so that we can do it.
…
Ian Williams, CDC [00:53:48]
Really the important underlying piece here, and the thing that really became clear to me during COVID, is really this idea of a source of truth around this data.
So how many cases are there today? And really sort of building pipelines and systems so that we can all agree on.
This is the number of cases and how we derived and got to that number of cases for this day. And really the idea here is this information needs to be able to be shared sort of across the entire public health enterprise so that we are transparent about where our data come from, how it becomes shared.
So really the idea is to develop and formalize and institutionalize sort of these base systems that that Matt Ritchey described here, and really like make sure that we’re clear on our data and data pipelines and that these pipelines are in place all the time, and we’re not developing them for each individual response, which has been sort of the tradition here at CDC, is every new response is a new day for us and we’re rebuilding these over and over again.
So it’s really important to make sure we have these and that this system that we’re building has flexibility to bring in new data and to integrate new data sources when we need it to sort of add and enrich the data that we have in front of us.
…
Matthew Ritchey, CDC [01:21:16]
I think it’s the more, the, not the better, but is it good enough?
Because I think when you get to better, it also is a slippery slope. And I think that gets us into bespoke systems and things like that, because you’re like, ‘oh, we could do this a little bit better to answer this one question.’ And it leads us down that pipeline, that path. And we know at the end of the day that doesn’t work for public health, right? It leads us in all the problems that were talked about through our colleague with the American Hospital Association, things like that.
So it’s about the multipurpose nature of it. And then in that, what’s good enough. And then how does it meet the timeliness needs and things that really help address the so what questions right. And how do we map that out ahead of time? Not in the moment.
Because when you’re in the moment, then MacGyver comes in and then you’re like just trying to piece it all together, right? So how do we try to get out ahead of it more and more, and actually that’s what we’re using this respiratory virus response for really in a lot of ways.
It’s a response that’s not a response.
Because I mean, right now we know that levels are not very high right now. We know they could be high, we could have another tripledemic, but it’s a really good moment to, while we’re like really in a concerted effort, bring these things together and be a little bit more thoughtful, instead of being in the moment of, ‘oh my gosh, we’re in a tripledemic right now, now what do we do?’
So we’re trying to balance it a little bit there.
September 28, 2023
CDC director on vaccines for fall respiratory season
- Source: webcast of National Foundation for Infectious Diseases press conference
- Date: broadcasted September 28, 2023
Mandy Cohen, CDC [00:28:35]
The good news here is that we have effective ways to protect ourselves from the worst outcomes of all of these respiratory illnesses.
Everyone six months and up should be getting their annual flu shot and the updated COVID vaccine, pregnant women, adults over 60, should be getting the RSV vaccine. Babies should be getting the updated– the new immunization for RSV. That should become available in the October timeframe.
So look, we have lots of tools, but I’ll just close again as a– not just the CDC director, but as a mom, as a wife, as a daughter, I wouldn’t recommend something for the American people that I wouldn’t recommend to my own family.
That’s why my 9 and 11 year old daughters are going to be getting their flu shot. They’re getting their updated COVID vaccine. My husband’s getting vaccinated. I already got my flu vaccine. I plan to get my updated COVID vaccine. My parents, again, getting vaccinated.
So I want to encourage everyone to join me in taking the time out of their schedule to protect themselves. It’s exciting we have these tools, we need to use them.
…
Mandy Cohen, CDC [00:47:25]
The first question on when is right now. I think that’s why we’re having the event.
We usually see the start of flu season, and as I already said, we’re already seeing an uptick in RSV cases, starting now.
We know on the COVID side that we have been having an increase in hospitalizations and cases. We had a late summer wave that we do actually see some declines in our hospitalizations in COVID, but we fully expect, based on what we’ve seen in previous years, that we’re going to see an increase in COVID as well.
So right now is the right time to be getting folks vaccinated, September and October, is that right time. So make a plan to do it.
And I would say, yes, get your vaccine at the same time, one appointment one and done, COVID and flu at the same time.
Again, those two vaccines are for anyone over the age of six months. For RSV, those are for particular populations. If you’re over 60, RSV vaccine for you.
The maternal vaccine, for RSV, was just recommended at the end of last week. So that is still starting to ship up out and be available. The immunization for babies is going to be available from the manufacturer in October.
So those are still ones that are rolling out, but for older adults, the RSV vaccine is available. You can get it now you can get them all on the same day.
Again is really your preference in terms of convenience.
…
Mandy Cohen, CDC [00:49:25]
On the shared decision making, the way that CDC made the recommendation was to have folks have a conversation with their doctor, their nurse practitioner, their pharmacist about the vaccine. And so, we frankly know that happens with most vaccines anyway, so I think this is, in certain places, we are seeing that there are certain requirements that are being put on.
So for example, here in the state of Georgia, the way they’ve interpreted that is for you to have a prescription for the vaccine. But that’s only in a few places.
Most of this is just a conversation so that folks can understand the vaccine again, because it is newer, that folks wanted I think the opportunity for folks to understand that vaccine and talk about it with someone. But frankly we know that that’s what happens across all vaccines.
So we encourage folks again, that’s why we’re here sharing this information, so you can go in with the best information to protect yourself.
…
Mandy Cohen, CDC [00:58:07]
We’re about two weeks into having the new updated COVID vaccine, and it is a different process this year.
So previous years this was– the vaccine was purchased by the federal government and then distributed by one entity. Now we’re sort of going back to what I’d call the normal course of business, the same way that flu vaccines are distributed, is the way these new updated COVID vaccines.
So it means that individual providers need to order them, the manufacturers and distributors need to ship them, and in ordering them, they purchase those vaccines. So again, it’s just a different process than we’ve done the last couple of years.
We do know that our manufacturers and distributors were getting out the adult vaccines first. So that was what was shipping, in the first number of days. And now they are shipping pediatric vaccine. We know pediatric vaccine has shipped.
We are seeing that shipped particularly to our Vaccine for Children program sites. Those are the sites where children and their families can get free COVID vaccines through that program.
So we know that it’s shipping. We know that they were shipping adult vaccine first and now pediatric vaccine.
So what I would say is that the supply is filling out, and make sure that you’re calling ahead to your pediatrician or your local pharmacy to see if the vaccine is available. And if not, check back again.
Novo Nordisk statement on Ozempic and ileus
- Source: email from a Novo Nordisk spokesperson
- Date: received September 28, 2023
Please see our statement below. Appreciate you updating your story.
“At Novo Nordisk, patient safety is a top priority. We work closely with the U.S. Food and Drug Administration (“FDA”) to continuously monitor the safety profile of our medicines. On September 22, 2023, FDA approved a label update for Ozempic® that added the term ‘ileus’ to the Postmarketing Experience section of the product labeling. Ileus is a gastrointestinal reaction that was reported in the post-marketing setting with Ozempic® and with other glucagon-like peptide 1 (GLP-1) receptor agonists.
Novo Nordisk stands behind the safety and efficacy of Ozempic® and all of our medicines when used consistent with the product labeling and the approved indications. For Ozempic®, the most commonly reported side effects include: nausea, vomiting, diarrhea, stomach (abdominal) pain, and constipation.
Full prescribing information for Ozempic® is available here.”
September 27, 2023
CDC officials discussing COVID-19 vaccines access
- Source: partial recording of conference call by Centers for Disease Control and Prevention officials
- Date: recorded September 27, 2023
CDC official [00:09:38]
Pharmacies are provided vaccine in a different way than public health clinics and infrastructure are.
Because pharmacies are receiving these donations through the reimbursement model, they have already ordered vaccines on the commercial marketplace, and are just being reimbursed for those that they use through the Bridge Access Program.
It does mean there’s not like a strict allotment number on any of these. And so, amount of vaccine that’s donated in any particular pharmacy will will vary by demand in that particular pharmacy, and will not vary by some sort of formal assignment, because again of this reimbursement model approach.
It is possible if manufacturers, as at least one has already indicated they will do, if manufacturers continue to provide donated vaccine as long as there is demand for it, it’s possible that we could see numbers continue to rise of donated vaccine on the pharmacy side.
However, just to reinforce again, this is not an a limitless program. This is a finite program with finite resources and at some point CDC will no longer be able to reimburse the cost of administration.
And so I don’t think anyone should think of either of these sides as being unlimited, either the public health infrastructure or the pharmacy side of the Bridge Access Program.
And I hope that the message that we can somehow take to our constituents from all this is don’t wait to get your no cost COVID 19 vaccine. If you are an uninsured adult, go ahead and get that now at a location that is convenient for you.
…
CDC official [00:13:42]
We’ve had an instance where, for example, people with Kaiser Permanente coverage go to a non Kaiser site and are told that either they need to go to a Kaiser pharmacy or just pay out of pocket for the vaccine. Those patients are not Bridge Access Program eligible. They do need to go to where they have coverage for their COVID 19 vaccine.
…
CDC official [00:15:16]
Once we recognized that Novavax wasn’t authorized, the new formulation wasn’t authorized, on the 11th of September, I think what our planning assumption has really shifted toward end of September, beginning of October.
So I don’t actually have updates about when it will actually occur, but I’ll just say that our planning assumptions are sort of looking toward end of this week, sometime next week, is when we think it might be likely that there’ll be an authorization.
But I mean, I know you know, this is an, an FDA decision and we don’t necessarily know the timing, but I just thought I would share what our planning assumptions are right now.
…
CDC official [00:20:07]
There is no residency requirement. There is no citizenship requirement. There is no documentation requirement. This program is meant to serve adults who are uninsured or underinsured, regardless of their residency.
…
CDC official [00:22:58]
There is this very specific group of adults ages 18 exactly who could be eligible either for VFC or for Bridge. And so just wanna acknowledge that overlap. And we’re kind of hoping, because of how limited the Bridge Access Program supply is, that providers with the option to use the VFC might consider using that.
But again, we don’t want to be directive. And we’ll just note that there are these 18 year olds who could be eligible for both.
…
CDC official [00:26:15]
In the retail pharmacy component of this program, our contracts stipulate that patients who walk in for example are just asked whether they have insurance or not.
It’s not a, a prove that you do not sort of situation, there’s no extensive documentation, it’s intentionally designed to be a very simple, low energy, low time consuming process because we want to reduce those barriers.
Now we also don’t want to fall prey to fraud in the background. In other words, putting the burden on pharmacy systems, they will first try to do insurance discovery, but this is all after service provision. So we want there to be no barriers for the patient. And we want all of the burden to fall on the systems that we have constructed to sort this all out.
And I think through this balance, we’re going to achieve low burden to patient, while achieving a lot of security in our own system.
So, and thus far it’s working very well.
…
CDC official [00:37:03]
That is currently the official end date of the program is December of 2024, or– would you add anything else to that?
CDC official [00:37:13]
The only exception would be if uptake was better than expected and we ran through all available doses and funding prior to that point, it would effectively end prior to that point.
In no case will it be– well not currently is it for foresee to exceed that point.
So it’s going to end by December 2024, regardless of what is used by that time.
FDA spokesperson in response to question about Ozempic
- Source: email from Chanapa Tantibanchachai of the Food and Drug Administration
- Date: received September 27, 2023
Although there is some overlap in the terms, ileus and gastroparesis, they are not synonymous. Ileus is a non-mechanical decrease or stoppage of the flow of intestinal contents. Gastroparesis is a chronic gastrointestinal syndrome defined by symptomatic delayed gastric emptying of contents into the intestine in the absence of mechanical obstruction. In addition to ileus, delay of gastric emptying is also mentioned in the United States Prescribing Information for Ozempic and other glucagon-like peptide-1 receptor agonists (GLP-1 RA).
The FDA monitors reports of gastroparesis and other related terms with GLP-1 RAs as part of our safety monitoring of a drug throughout its life cycle, including post-approval. In addition, the FDA maintains a system of postmarketing surveillance and risk assessment programs to identify and evaluate adverse events that did not appear during the drug development process. If newly identified safety signals are identified, the FDA will determine what, if any, actions are appropriate after a thorough review of available data. For additional information, please refer to the following:
https://www.fda.gov/drugs/questions-and-answers-fdas-adverse-event-reporting-system-faers/fda-adverse-event-reporting-system-faers-public-dashboard
CDC official at webinar on RSV immunizations available
- Source: webinar by Centers for Disease Control and Prevention
- Date: broadcasted September 27, 2023
Jefferson Jones, CDC [00:42:18]
So regarding supply of these products, there is no anticipated supply demand mismatch.
However, because the Pfizer maternal RSV vaccine, in addition, the Pfizer maternal RSV vaccine is the exact same product that has been approved for use in adults aged 60 years or older. And so availability is expected now that we’re at after ACIP recommendations. However it may, for those that are asked in obstetricians or other clinics, that may not store the vaccine previously, some time may be required.
Now nirsevimab, shipping has begun and availability is expected either in by late September or early October, but it may not be available in all pediatric settings this season and efforts are underway to increase the number of birthing hospitals who will administer nirsevimab.
…
Jefferson Jones, CDC [00:44:47]
So there’s no official announcement that comes out each year by CDC.
This year, a health alert network was released encouraging uptake of RSV vaccines, and nirsevimab as soon as it becomes available, as we are seeing RSV transmission this season, similar to pre pandemic transmission, which means we’ve seen it begin in Florida and it appears to be spreading in the south and we expect it to spread to the United States.
If it follows pre pandemic seasonality, it peaks in December through February, but one dose of nirsevimab gives at least five months protection. And so really the target is shortly before the start of the RSV season, which generally starts in, in mid to late October in the majority of the United States, are slightly later in the Western regions.
So recommendations are to, on a yearly basis, to begin administration the beginning of October, if there are for certain territories and states, there may be more regional specific recommendations from local health authorities, and if those are available, those should be followed.
…
Jefferson Jones, CDC [00:50:32]
So there is no preferential recommendation.
Caution should be urged when comparing the efficacy estimates of the maternal vaccine studies and the nirsevimab studies, as they were not head to head, they were different populations, different times of year, and most really importantly, is different outcomes.
While they both had medically attended RSV LRTI and RSV associated hospitalization, there were some differences. And then the trials for nirsevimab didn’t have an equivalent severe RSV, which was the definition in the maternal vaccine.
There is reason to believe that protection from nirsevimab may last longer, as the monoclonal antibody has been engineered to, in the constant portion of that antibody, to have a much prolonged halflife compared to standard antibodies that are passed through the placenta. So that is something that could be considered. Clinical judgment is always warranted. Clinician judgments should be shared with their patients when discussing.
But CDC and ACIP did not have– make a preferential recommendation.
I think most importantly is to say there are two options. All infants should be protected through one of these options. And both options should be considered at the time of pregnancy.
And one thing I would add for those that are, I do know of people that look at the data and feel pretty confident that they, prefer under nirsevimab based on the levels of efficacy and the studies, and just there are issues with potential availability this season.
And so one thing just to consider is if declining the maternal vaccine in order to use nirsevimab for that infant, trying to confirm that nirsevimab will be available for that infant would be ideal.
…
Jefferson Jones, CDC [00:53:24]
So both RhoGAM and other antibodies– I mean, same thing has been asked, could nirsevimab interfere, could actually make it worse by giving nirsevimab after maternal RSV vaccine?
And because antibodies are targeting a specific antigen, RhoGAM would not be expected to interfere with the maternal, with any maternal vaccine, whether it’s flu, COVID, Tdap, or RSV, as it’s targeting a very different antigen than, and not targeting other antibodies. And the same would be for giving nirsevimab after maternal RSV vaccine that, it wouldn’t be expected to interfere, because the antibodies target the virus specifically the, in the case of nirsevimab, the F protein and not other antibodies.
California health department officials on COVID-19 vaccines
- Source: webinar by California Department of Public Health
- Date: published September 22, 2023
Alan Hendrickson, California DPH [00:13:37]
Novavax, the old vaccine or non updated vaccine, continue to administer that.
What’s up with Novavax?
Just got an email this morning from our rep there. And, she said, there’s still playing question and answer with the FDA. So hopefully there’s a– we will have updates for you early next week on where they are on that vaccine.
Also on the Novavax, there was an error in the product guide, which we updated, thank you to April.
The BUD for those punctured vials is six, not 12 hours, I guess that was wishful thinking on my part.
…
Edward Salaguinto, California DPH [00:45:20]
To fill in the other gaps, eTrueNorth has enrolled other community pharmacies intended to reach lower access areas without other coverage.
eTrueNorth is still actively trying to enroll more pharmacies. They did tell us that currently there’s some legal reasons why they can’t include some of the other larger chains. And that includes Rite Aid, the Kroger group, Albertson, Safeways, among others, even Walmart. So they couldn’t tell us why, but smaller chains weren’t excluded. So smaller chains are still trying to be outreached.
…
Edward Salaguinto, California DPH [00:47:16]
Some of you may have noticed that that claims have been rejecting for Medi-Cal.
Medi-Cal is aware of this and all COVID 19 formulations are already added to the contract drug list, behind the scenes.
But, back in January of last year, Medi-Cal contracted with a third party adjudicator, Magellan. Magellan is currently uploading those files and also Medi-Cal working on some of their– just some of what they need to do behind the scenes.
So hopefully this will start adjudicating properly sometime next week. But we’ve seen this like previously when other vaccines were introduced.
There is a communication that DHCS issued late yesterday, and I just received this and it does explain all this.
…
Maria Volk, California DPH [01:12:56]
I just wanted to talk about ordering for the BAP program for just a second, and our allocations.
So I know we’ve shared that, in our communications, that we have received very limited allocations, especially for Pfizer. So we’re doing our best to approve orders, but know that we have not been able, across all of the local health departments, to approve all of the orders that have come in.
Just to give you a sense of the numbers, we got 4,500 doses of Pfizer and 35,000 doses of Moderna. So that Pfizer number is very, very small.
We do know that CDC was meeting with Pfizer this week to try– actually both the manufacturers to try and understand how doses are rolling out, what to expect for allocations, and the timelines. So we hope to have more information to share with you next week.
But just want to acknowledge that, especially on the Pfizer side, it’s rolling out a little slow. I mean, we think that those doses should be available soon and we’ll be able to replenish allocations and this will get easier.
But I think as we all probably expected, a little bumpy coming out of the gate, with the doses that are available.
…
Claudia Aguiluz, California DPH [01:14:43]
So we actually did open up ordering for VFC program providers early this week. So vaccines are now in your order form, you will see that orange segment in your order order form, and you would also see that Moderna for pediatric patients six months through five years, it is also available for ordering, we did receive supplies of that vaccine at McKesson. So just wanted to encourage providers to go ahead and place orders.
CDC officials at summit on public health data issues
- Source: webcast of CDC Health Data Innovation Summit
- Date: broadcasted September 27, 2023
Mandy Cohen, CDC [00:01:22]
I’m a data gal at heart.
Data is the oxygen that powers our ability to detect and respond to threats. It’s the entire mission of why the CDC exists, and it’s such a critical asset for our country.
And I’m super grateful to see so many friends out here and data leaders.
…
Mandy Cohen, CDC [00:03:55]
One of the first things I focused on here at CDC was honestly to change our mindset around data.
Unfortunately, and I’ve shared this at our all staff meeting, and so this is stuff I share with our team, I can’t tell you how disappointed, how many times I’ve unfortunately heard the phrase, ‘Well, that data is mine. Well, that’s our center’s data. That’s our team’s data.’
And they’re very good data stewards, right. They work hard to collect that data. They know it inside and out better than anyone else.
But just because you are the collector or the steward of that data, it does not make it yours. Public health data is that critical national security asset that needs to be available, appropriately available, with context, it needs to be available as widely as possible to help us navigate the known and unknown future health challenges we face.
And so I know our teams want that data to be explained in the highest degree and everyone to understand it, but we have to make it accessible to folks who don’t have a background in data science, who don’t have a background in public health that want to understand what’s happening in their community so that they can make good, common sense decisions about how to protect themselves.
That’s what we need to do. And it’s the challenge we face ahead. And so that starts here at CDC, but it’s not, that is not the end of the story. This has to be a two way street. Just as CDC needs to move away from this data is mine mentality, so do all of our partners, whether it’s our state partners, local governments, tribal authorities, you all have critical data. And I include our healthcare system in that.
That our nation needs to protect health beyond the borders of your health system, beyond the county, beyond the state, beyond the locality, we need to work together to figure out how to get that data to flow.
…
Mandy Cohen, CDC [00:07:39]
We need to get aligned in what we are doing in our approaches to this work.
We cannot build one offs anymore. We are an integrated matrix, complex, messy, but importantly strong together asset. And we need to make sure that we are aligned in the overarching strategy, the priorities and the standards.
So no more one offs, we’re on one team, but it means we’re gonna have to partner in different and better ways and that communication and that collaboration is starts here.
…
Jennifer Layden, CDC [00:08:56]
As you look at this org structure, you’ll see a couple things, that there are five divisions. Those are the five listed on the bottom.
Those five divisions are focused around the core missions of public health. So we spoke to it and Dr. Cohen mentioned that as well, as we really wanted to emphasize the importance of what we’re doing, what the data is serving.
So the importance of public health to be able to monitor and detect threats, whether they’re new threats, they’re evolving threats, they’re aberrations, and known chronic public health threats. We are not per se the office that is doing that monitoring detecting. We are enabling it to be done better across public health, whether it’s at CDC or with our state, local, tribal, territorial partners.
Similarly, a core role of public health, investigating and responding. So how do we investigate and respond? How do we develop technology solutions to support the ability of our state and local partners to investigate and respond to public health threats?
And then our responsibility to inform and disseminate, get data and information out there to different audiences in using different and evolving and emerging ways to get that data and information out there.
So our structure was really aligned to the mission. What is the mission that we within public health need to do, and then structure our org structure to enable us and to really emphasize the importance of not just the data, but the technology that we are prioritizing and building.
You’ll see, importantly, that there is a division on platforms and we’ll have our platform lead to talk about that, as well as on data policy and standards.
…
Matthew Ritche, CDC [00:29:58]
Our actionable data branch is really focused on how do we leverage data, get it positioned and analyzed in a way that helps inform action.
Our sister branch is our dissemination technology and services branch. This then takes it that last mile. It then says, ‘okay, we have actionable data, actionable data products that have been developed, whether within our own specific division or by other divisions within our office, or even across the agency. And how do we position that for different audiences so that it actually is meaningful that we actually meet the mark? We communicate what we think needs to be communicated to inform people’s behaviors, or at least hopefully informs their behaviors?’
So a big part of that right now is our support of the respiratory viruses response.
So it’s a center-led response center at our agency looking at a pan respiratory model, as far as not looking just at COVID, not just at flu, not just at RSV or other respiratory diseases, but how do we look at them collectively, but then also be able to bridge into information that’s specific to each one of those condition types.
So our division has been very invested in helping support this overall response, and we’re supporting the response to get kind of to achieve that mission, but we also have a bigger agency mission in mind as well. So that bigger mission for the agency is not just like, ‘Hey, we have one specific response that we need to be able to share information out about,’ but how do we create enduring capabilities that the agency that allows us to lift and apply to future responses, future other programmatic efforts, especially when those programmatic efforts require a lot of coordination across different groups at our agency.
…
Matthew Ritche, CDC [00:31:40]
So one of the big efforts that we’re doing right now in the dissemination side is a project that we’re calling Sapphire. And what Sapphire stands for is Sharing Ationable Public Health Information in a Responsive Environment.
So a big idea about this is how do we package information, put it out for public display, whether on our website or other mediums or other platforms, and again, making it responsive to the end user. So a big part of that, and Michael mentioned it earlier, is this idea of human center design. And that’s a big component of what we’re working into specifically this branche’s activities.
How do we involve the intended end user, the audience, into the design process? It could be a program. It could be somebody in the general public. It could be some of our other partners.
How do we from the get go bring them into that design process so that when we get to that final product, they’ve been a part of that from the get go and it meets the need for them.
So that’s been a big part of what we’re doing for the respiratory virus response and ultimately what we’re trying to build again, as an enduring capability, for the agency.
…
Michael Radwin, CDC [00:43:03]
I’m new to government and I will confess that I am a little frustrated with in fact just how waterfall things are.
We have teams that are Agile teams using either Scrum or Kanban, two of the really popular Agile methodologies, but instead of shipping software every two weeks or actually multiple times a day, which is sort of what I’m used to, we’re a little slower on the shipping and part of the problem has to do with what I would call central central and cloud hosting versus distributing software through sort of older mechanisms.
So part one is how do we move away from packaging up software used to be that we would put things on CDs or DVDs, like burned software on and then sell it at Costco or Walmart other places, and then you’d go and install it, and we’re actually still doing that quite a bit with public health software.
When you think about case surveillance systems, whether it’s MBS, which we develop, or it’s it’s Epi-Tracks or it’s Maven or Clinisys or some of the other systems that are there, they’re packaged software. And actually really the model we need to move to is hosted software.
And we’ve done some of these, there’s some good examples of this. I think things like the AIMS platform and ReportStream, these intermediaries that do routing, really, really excellent example of cloud based centralized software. And it’s– that’s how modern software at companies like Jorge and I worked at before. That’s how we developed software.
You have the same team that is engineering the software is actually hosting it, and there’s just a lot more cost efficiency there. A lot more agility as data volumes surge, it’s very easy to scale up, because of these sort of elastic computing environments and just the overall operations cost, instead of having 15 or 20 or 64 copies of the software running, you really have one copy of the software running and that gives you some economy of scale.
The second thing I’ll say, and then I’ll let others chime in, is around what an approach we use called Strangler Fig, which is a funny name.
There’s a tree that occurs in nature where there’s a living tree. And then there’s this like a fig tree that kind of grows around the original tree. And that’s the– that’s a metaphor for what we do with modernizing systems in a way that delivers incremental value.
So what, if you go heads down and spend a year or three in a very waterfall way, trying to build a new version of whatever it is that you’re trying to do, then you aren’t delivering any value to the end user incrementally.
The Strangler Fig approach says we’re going to use, we’re going to build an entirely new version of software, sort of on the side. And we’re gonna put a router, a proxy, a widget in front that at first sends a hundred percent of the traffic or the request to the old thing. But over time as we build up new functionality, week by week, day by day, then a greater percentage of the product gets served out of the new modernized system.
And eventually over time, much like the strangler fig itself actually sort of becomes the new tree, the new modernized application becomes the primary thing. And then you can eventually shut down the old app.
It actually takes longer, I think, to develop software in this way and that using this Strangler Fig approach, because you have to keep the old version and the new version running simultaneously, however, it’s, I believe the best way to deliver incremental value to the users without breaking anything.
And so you can– we can ship these incremental updates along the way.
HHS official on impact of shutdown on Medicare drug price talks
- Source: email from HHS official
- Date: received September 26, 2023
Please see below on background:
The Secretary was noting that while core staff will still be working towards meeting the milestones laid out in the Inflation Reduction Act on the negotiations over the top ten Medicare drug prices, support and many career staff across CMS will be furloughed. Shutdowns are disruptive and distracting, making it difficult for agencies to deliver for the American people at the same pace—even for programs with available funding—given how much time and attention must go to managing the impacts of a shutdown.
September 25, 2023
CDC officials and NVAC members on fall respiratory virus season
- Source: webcast of National Vaccines Advisory Committee meeting
- Date: broadcasted September 22, 2023
Sara Dodge Ramey, CDC [00:21:59]
We are conducting research using multiple mechanisms, working with the division, center, and agency. Our goal is to gain insight on knowledge about specific topics, learn which terms best resonate with various audiences, inform our messaging and develop best practices. Next slide please.
In anticipation of the upcoming 2023-2024 cold and flu season, CDC conducted focus groups to better understand how people think about viral respiratory diseases and baseline knowledge, attitudes, and beliefs in order to inform our communications. There were a total of 12 virtual focus groups, which included general population and parents between June 27th and July 13th of this year. Participants were screened for a mix of health insurance type, gender, race, ethnicity, and educational attainment.
Some of the findings included a lack of knowledge and general uncertainty as to what a viral respiratory disease was. Specifically, which diseases were viral rather than bacterial. And what that meant most assumed that a viral respiratory disease was anything related to the lungs, including pneumonia, COPD, asthma, and even strep throat. The term viral respiratory disease season seemed long unnecessary and an escalation that felt scary to many.
Most participants preferred “flu” or “cold and flu” season or “fall and winter.” Many participants thought flu season was a catchall phrase that included a range of illnesses, not just flu.
A portion of participants reported COVID 19 fatigue and more hesitancy to being concerned about other disease. And the knowledge of RSV was low overall, but there was more concern among parents, though a few older adults also expressed concern. Most participants were open to talking RSV, even if they didn’t want to talk about flu or COVID.
…
Sara Dodge Ramey, CDC [00:23:51]
Participants approached prevention to viral respiratory disease as taking a blanket defense rather than anything else specific. There was little distinction between preventative actions for viral respiratory diseases versus non respiratory infectious diseases.
The most common prevention methods were related to a holistic approach to health, like eating well, taking vitamins, and exercising.
When sick, participants reported taking precautions to avoid spreading their illness, including staying home when sick, keeping their children home, using masks in public, and using hand sanitizing.
Some participants felt that the list of preventive actions where things they already knew, but stated there are people that didn’t know them and should learn them. Other participants liked the list of prevention actions because it reaffirmed what they were doing was right.
…
Sara Dodge Ramey, CDC [00:24:40]
Vaccines were not a top of mind preventive action for most. Many considered them to be a lower priority than everyday common sense measures.
There were mixed feelings about vaccines. Some were adamant about getting all recommended vaccines. Some believed they were ineffective or unnecessary, with most landing in the middle of the two extremes.
Most participants thought an effective vaccine prevented illness entirely. Some understood a vaccine could lessen the severity.
When vaccines were included in a list of prevention activities, some people pointed out that listing it first could detract from the value of the list, although they would be okay with seeing vaccines somewhere on the list, just not first.
…
Sara Dodge Ramey, CDC [00:25:29]
In general, people prefer softer language around vaccination recommendations when coming from CDC.
We know that a strong recommendation is effective when it comes from a healthcare provider. As such, we often play around with different calls to actions, like talk to your doctor, find out about where to get vaccinated, or talk to your doctor about X vaccine.
Educational messaging is a door opener. We have found that people preferred simplified, brief information, but enough that they feel that they have enough to take action.
Generally, we want to try and incorporate brief messages about risk, why the vaccine is needed, what the beliefs are or the benefits are, and where they can go to learn more.
Again, they like to feel empowered, to learn more and do their own research versus being told what to do
…
Sara Dodge Ramey, CDC [00:26:11]
Avoid messages that could be seen as a scare tactic, set realistic expectations.
People are more likely to perceive messages as credible and trustworthy if they set realistic expectations about what vaccines can and cannot do.
This is one reason why our flu campaign’s “Wild to Mild” concept performed so well in testing.
It clarifies that people can get flu if they’re vaccinated, while emphasizing that the vaccine still offers benefits even if you get sick.
…
Sara Dodge Ramey, CDC [00:27:23]
The back to school childhood vaccination campaign kicked off the week of July 10th with campaign materials deployed in partner engagement, toolkits disseminated.
The flu campaign had a soft launch of their digital assets in market in mid-August, with a media event on September 6th with the CDC director, and the kickoff being September 28th.
The campaign runs mid-August through February of 24, where the focus being on parents of children, 0 to 17, and pregnant people.
…
Sara Dodge Ramey, CDC [00:28:24]
NCIRD is also working on activities around a general pan-respiratory season, which includes flu, COVID 19, and RSV.
The plan is to kick off in October to the general adult public, including families and older adults and healthcare providers. We currently have materials in testing and development, including healthcare providers, specific outreach, social media, digital video spots, and the development of a partner toolkit.
…
Mitchel Rothholz, APhA [00:31:44]
Just reiterating what was just said in terms of payers who aren’t updating their systems. For example, with COVID, they’re still treating it in their system as if the government was providing the vaccine and haven’t changed over the commercial. And it’s causing a frustration by patients and the providers, patients ready to get vaccinated and providers concerned about being stuck with the money like they have in other programs.
And Bob, I just want to reiterate the point you made on RSV, because we’re seeing that a lot and not only from a payer perspective, but from authority at the state level, at least for pharmacy, in some states they require it to be published on the schedule for pharmacists to be able to do it.
So there’s a delay there and that’s why I called the other day for a look at the implementation process. Once something comes out of CDC for recommendations and, again, reiterate the need for a buffer so that we have time for implementation.
Manisha Patel, CDC [00:32:38]
And I’ll just add the specific question about the barrier for the schedule is being addressed this afternoon at ACIP as well. And so we do expect at least that barrier to be removed, but I anticipate there’s gonna be ongoing barriers from the actual frontline.
Mitchel Rothholz, APhA [00:32:56]
Yeah, I thank you for that. And I think the other part is, looking at, from CMS and the administration of what other, I wouldn’t call it enforcement, what other encouragement can the government give to the plans who are– they’ll say they’re covered under ACA, but if you’re not an in network provider, if you’re not in their list, then they don’t cover it. So that becomes a barrier as well.
So I think not only that the guidance that CDC and CMS put out earlier about being able to start implementing, a lot of– a good number of plans did not even follow that. So there needs to be some stronger enforcement to put that in place, unless we’re going to continue to face these obstructions.
…
Robert Schechter, California DPH [00:36:38]
I did have just one comment on the Bridge Access Program is that while doses have gotten out there, they aren’t out as widely as an expectation that, from some of the messaging, that that vaccine is available broadly.
And I realize that that’s a hiccup that we’ll get solved in time, but I think it reflects a challenge of trying to capture early interest when supplies may not be able to meet all that interest or result in the frustration of having to call around to a number of places or locate that available supply.
I did want to ask you for clarification of which aspect, which barrier of RSV vaccine, or nirsevimab, you expect to be addressed today at the ACIP meeting. I didn’t quite catch which aspect of that, and also a plea for what can be done to incentivize or, payers to cover cover nirsevimab as quickly as possible.
Hearing now from both our birth hospitals in the state of California, some of which are– many of which are reluctant to bear that that cost before reimbursement, similar concerns on the outpatient side. And I can imagine the same for prenatal providers for the RSV vaccine.
And so, shared reluctance and wondering what the other partners in the mix are going to be doing, and seeing RSV season coming upon us shortly, if not here already, and wondering how to protect as many infants this season as possible.
…
Manisha Patel, CDC [00:38:48]
One challenge though, is that most hospitals and Dr. Schechter, you might actually know this already, is that they’re not VFC providers.
And so how you onboard birthing hospitals is a challenge. The product availability, we don’t have it on the shelves yet. It’s supposed to be available in the next couple of months, but we’re already entering RSV season as you know, Florida and the Southeast is already seeing increased an uptick in RSV disease activity. And so some of the other sort of barriers I also think is just the communication around nirsevimab versus maternal or RSV vaccine for pregnant people.
And if there’s going to be insurance coverage issues, if a mom got RSV maternal vaccine, but we don’t have records. And the pediatrician’s not sure now what to do about nirsevimab.
So there’s a list of different things that many folks are working through. And, I think the earlier question you had about what’s being discussed today, I’m trying to remember what I said that made you think that, but the one thing is just that all of this stuff that’s going to be on the actual immunization schedule, all of these different new recommendations, updated sooner than the typical updates in the spring, I believe.
September 22, 2023
CDC committee meeting on Abrysvo in pregnancy, new vaccine schedules
- Source: webcast of Advisory Committee on Immunization Practices meeting by the Centers for Disease Control and Prevention
- Date: broadcasted on September 22, 2023
Malini DeSilva, HealthPartners Institute [10:29:23]
The goal is to evaluate the safety of the RSVpreF vaccine administered during pregnancy in the VSD’s large real world population.
Challenges of the surveillance work include unknown vaccine uptake, which makes it difficult to provide any power estimates.
Additionally, we may see a healthy bias, where healthier individuals or those with lower risk pregnancies may be the first to be vaccinated.
This will be considered in our analyses and when interpreting results.
There is uncertainty regarding recommendations for use in administration of this vaccine, which may impact who receives the vaccine.
If persons at high risk for preterm delivery are recommended to receive RSVpreF early in the vaccination window, we may identify more preterm birth in our vaccinated group. Alternatively, these individuals may be counseled to not receive the vaccine and wait to have their infant received nirsevimab.
The timing of administration during pregnancy overlaps with Tdap recommendations and vaccinating administrations are also likely to overlap with influenza and COVID 19 vaccines.
Coadministration of RSVpreF with other vaccines will be taken into account in our analyses.
…
Malini DeSilva, HealthPartners Institute [10:30:55]
Our primary approach for prenatal RSVpreF surveillance will be through bimonthly surveillance.
We’ll use validated algorithms applied to electronic health data in the VSD population to identify pregnant persons 16 through 49 years of age, at 20 weeks gestation or later.
We’ll exclude pregnancies ending in therapeutic abortion, multiple gestation pregnancies, and those with insufficient information to determine the start date of the pregnancy.
The exposure we are evaluating is RSVpreF vaccination at or after 28 weeks gestation. This is to account for any inaccuracies in gestational age estimation.
We plan to match pregnant persons vaccinated with RSVpreF to pregnant persons unvaccinated one to one, based on VSD site and gestational age at vaccination.
We will create propensity scores to account for confounding using readily available variables, such as pregnant person’s age, pregnancy start date, race, ethnicity, and medical comorbidities.
…
Malini DeSilva, HealthPartners Institute [10:35:36]
This slide shows an example timeline for our planned bimonthly surveillance.
If vaccinations start in October, we would plan to capture two months of vaccinations followed by a 42 day follow-up period and two month data lag before pulling any data.
Our first data pull would be in March of 2024.
We will continue bimonthly surveillance every two months.
…
Pedro Moro, CDC [10:37:59]
For more than a decade, VAERS has been used as part of vaccine safety surveillance for vaccines used in pregnancies, such as influenza Tdap, and COVID 19.
So one type of analysis is a descriptive analysis, which includes clinical review of individual reports, aggregate descriptions of automated data, which involves counts of reported adverse events, and also calculation of reporting rates for pregnancy outcomes. And this can be done if there are doses of RSV vaccine administered in pregnancy, or if there’s data on vaccination coverage.
Now statistical analyses may be done. Historically the approach has been to use data mining to assess for disproportionate reporting. And this is under discussion right now for RSV vaccines.
…
Pedro Moro, CDC [10:42:39]
Now with regards to be V-safe, there is a new version of V-safe, developed starting the summer of 2023. And this system leverages existing CDC IT infrastructure. It includes email and text messaging options and is the first use for RSV vaccines received by persons age 60 and older. And use of maternal RSV vaccine is planned to be monitored later this fall.
V-safe objectives include characterization of local and systemic reactogenicity during days 0 to 7 after vaccination, characterizing health impacts during a six week post vaccination follow up period, and also identify participants who report medically attended events after vaccination and encourage completion of adverse report.
…
Katherine Poehling, ACIP [10:44:13]
In the Vaccine Safety Datalink is how are you planning to handle pregnancies with multiple gestations? The twins, the triplets, etcetera, as they are at risk for additional preterm births? Thank you.
Malini DeSilva, HealthPartners Institute [10:44:35]
Thank you. We, for this initial planned evaluation, we have excluded them. As you mentioned, they are at higher risk for preterm birth. We are planning a more comprehensive in-season evaluation, and we’ll consider how to account for multiple gestation births in that as well.
…
Anne Hause, CDC [10:45:51]
So the new version of V-safe is still in the final stages of development.
We do plan on launching this fall and evaluating the RSV vaccine for older adults first. And then later this fall, we hope to launch for the maternal RSV vaccines. So no data yet.
…
Grace Lee, ACIP [10:46:25]
Nothing of note from VAERS regarding the older adult population? I’m guessing we haven’t had enough doses in, but Dr. Shimabukuro, if you could just let us know? That’d be great.
Tom Shimabukuro, CDC [10:46:37]
We’re monitoring and we are receiving reports, a small number of reports, but we haven’t seen any unusual or unexpected patterns at this point.
…
Beth Bell, ACIP [10:47:06]
So I’m wondering if anybody’s done any back of the envelope calculations using different assumptions for uptake, understanding what you would expect in terms of accrual of pregnancies in your database and, various estimates of power and such, to give us some sense of how long you think it might take, depending on what happens with uptake to, have some useful results from the VSD? Thank you.
Malini DeSilva, HealthPartners Institute [10:47:35]
At this time with the uncertainty about the vaccine uptake, and while we’re awaiting recommendations for use, we anticipate we’ll be well powered to detect significant differences in pre-term birth within six months of vaccine eligibility.
Additionally, we are planning to perform some preterm and still birth surveillance that will be separate from this planned bimonthly surveillance.
This would only be descriptive, and while it’s descriptive, it would be limited to the vaccinated population, it can be formed— we perform slightly more quickly, but that, it would be needed to be noted that these results will lack a control population, still require a data like similar to similar to other VSD work, and would not include any statistical comparisons.
So, it’s still going to be a little bit of time, but we do think we’ll be well powered within six months.
…
Ruth Link-Gelles, CDC [10:54:32]
So we have a number of plans in place to study post licensure effectiveness of maternal RSV vaccine. And we work closely with the group here at CDC.
I will say generally, getting one vaccine is predictive of getting another vaccine. So it becomes very difficult to find people who got only pertussis, for example, or only RSV.
So looking at co-administration, with real world data can be difficult, but we do have a number of plans in place to attempt to do that.
…
David Hutton, University of Michigan [11:00:13]
The other big update here is that we’re using a $295 per dose cost. That is an increase from the $200 a dose estimate we had in June.
So it’s a significant increase in the price per dose.
…
David Hutton, University of Michigan [11:07:23]
So this is just assuming that none of them will be receiving nirsevimab.
So in the next slide here, I just want to recap the summary, RSVpreF may improve RSV outcomes, but also will increase costs. RSVpreF has the potential to be cost effective, and results are sensitive to a wide variety of assumptions.
…
David Hutton, University of Michigan [11:16:54]
If you know the babies are gonna receive nirsevimab, there’s very marginal additional benefit beyond that nirsevimab protection that’s conferred by RSVpreF protection, and these incremental cost effectiveness ratios are extremely high.
So just, in the next slide here, I just want to recap some summary here.
Limitation, I want to highlight again, there’s no efficacy of data on these combined products, so these are all based on assumptions about what the efficacy might be.
Nirsevimab may add additional protection on top of RSVpreF, particularly for high risk infants, and then adding RSVpreF on top of nirsevimab does only really add marginal effectiveness at a very high cost to the population.
…
Donna Altenpohl, Pfizer [11:43:43]
The Abrysvo WAC price is $295 a dose for both the maternal and older adult indications.
Because the Pfizer RSV vaccine is the same product and the same formulation for both indications, it has one NDC code and one CPT code for reimbursement, requiring one price for both indications.
We took this into consideration, as Pfizer’s pricing strategy is guided by the value that our innovation brings to patients in society with the goal of achieving the broadest possible access for patients.
Based on the results of our cost effectiveness analysis, we priced our vaccine to be both cost effective and reflect the value it’ll bring in helping to prevent RSV for older adults and infants.
As we shared the ACIP working group, the RSV maternal vaccine will be a lower cost option and could result in a lower budget impact to the U.S. healthcare system.
…
Katherine Fleming-Dutra, CDC [11:47:35]
Just to add to that and to your point as well, we do have data from other vaccines, such as Tdap, flu, and, influenza vaccines and COVID vaccines, which does indicate that effectiveness, post maternal vaccination of other vaccines, has usually has waned by six months as well.
…
Pablo Sanchez, ACIP [11:48:46]
My comment is related to the vaccine price. And I’m really very disappointed about the expense of this vaccine when a recommendation may be made to provide it to all pregnant women.
And I would like to know what is the cost of this vaccine countries outside the United States, and is it being priced— are we being overpriced?
And for instance, in Europe, do they know what is the price there? It has to have been a standardized price throughout the world? Thank you.
…
Jessica Atwell, Pfizer [11:49:55]
So we wanted to provide a little bit more context into the data that inform the waning assumption, or antibody persistence in infants beyond six months.
So in addition to the data from our phase 3 clinical trial, we also have data from our phase 2B study that measured antibody persistence in infants out to six months. And compared those levels between infants born to vaccinated individuals and unvaccinated individuals.
They were significantly higher compared to among infants born to vaccinated individuals, compared to infants who was born to women who received placebo in the phase 2B.
We used the half life of antibody decay from those data to then extend the potential antibody persistence beyond the six month time point. And that modeling, which was shared with the work group showed persistence even beyond nine months out to 12 months.
Of course, there is no correlate of protection for RSV, and so it is difficult to make direct assumptions about what those antibody levels may translate to, but we certainly have data to support persistence in infants beyond six months.
And that was really critical for informing this assumption about persistence of antibodies and potential benefit.
…
David Hutton, University of Michigan [11:53:21]
And there are a lot of different things kind of going on here. I think a big thing is in our simulation modeling of nirsevimab, the efficacy is slightly better at the beginning, and so slightly higher efficacy. So that’s one difference.
And then the other difference too, I think is, that nirsevimab can be given to kind of time right at the peak of the RSV season. And that’s kind of the idea there is, so if a child is born in April, May, June, July, for example, they would be given nirsevimab to have that kind of peak efficacy during the season.
And so I think those are a couple of things that affect the differences in cost effectiveness of nirsevimab versus the RSVpreF, what you’re seeing here today on RSVpreF.
David Kimberlin, AAP [11:54:14]
And so remind me then of, when in your presentation where you did kind of group together the months, so you had different seasons, are we toward 100,000 per QALY for timing maternal vaccination when it’s just a bit before or during RSV season?
David Hutton, University of Michigan [11:54:35]
Yeah, exactly. So the cost effectiveness of RSVpreF looks much, much better when it’s given kind of right before the peak of the RSV season, because then it will confer the highest levels of efficacy during that peak of the seasonality.
And so that’s a big factor there as well.
…
Donna Altenpohl, Pfizer [11:57:02]
We have a tiered pricing strategy outside the U.S., which allows the price to be contingent upon the affordability of each individual country, as we’re beginning to launch the RSV maternal vaccine. The pricing will be decided at that point.
…
Katherine Fleming Dutra, CDC [12:11:08]
And I have highlighted the dosing window of 32 through 36 weeks gestation here, because this is a change from the policy question that we discussed at the June ACIP meeting. And throughout the presentation, the highlighted text denotes, key points and information, which have been updated since June.
As Dr. Long has already discussed, the reason for this change is because FDA approved the Pfizer RSV vaccine for use in pregnant people as a single dose to be given at 32 through 36 weeks gestation to avoid the risk of extremely preterm births, where there is substantive, morbidity and mortality, and very preterm birth.
FDA considered the benefit of vaccine efficacy when the Pfizer RSV vaccine is administered between 32 and 36 weeks outweighed the risk of vaccination, including the potential risk of preterm birth and hypertensive disorders of pregnancy.
As a reminder in the phase two B and three trials, vaccination was given during 24 through 36 weeks gestation. So throughout the presentation, I will refer to the approved dosing interval of 32 through 36 weeks gestation. And the trial dosing interval of 24 through 36 weeks gestation.
…
Katherine Fleming Dutra, CDC [12:12:54]
RSV infection is the leading cause of hospitalization in U.S. infants. Most infants are infected in the first year of life and nearly all by age two and 2 to 3% of young infants will be hospitalized for RSV.
It is a common cause of lower respiratory tract infection in infants, and the highest RSV hospitalization rates occur in the first months of life.
And all young infants are at risk of severe disease with RSV. 79% of children hospitalized with RSV aged less than two years had no underlying medical conditions.
When asked is RSV among infants of public health importance, the work group unanimously responded. Yes.
…
Katherine Fleming Dutra, CDC [12:14:51]
As a reminder, vaccine efficacy against medically attended RSV associated lower respiratory tract infection in infants was 51% and efficacy against hospitalization for RSV associated lower respiratory tract infection in infants was 56.8%.
Additional data received since June are highlighted. These include the important outcomes of ICU admission for RSV hospitalization and infants, which had an efficacy of 42.9%, and mechanical ventilation, with an efficacy of 100%. But both estimates had very wide confidence intervals, and thus the certainty assessments were downgraded with very serious concerns for imprecision.
Additionally, we now have data for all cause hospitalization for lower respiratory tract infection with an efficacy of 28.9% with a confidence interval that crosses the null and thus a certainty assessment was downgraded for serious concern for imprecision.
…
Katherine Fleming Dutra, CDC [12:15:54]
Specifically, we have now downgraded three outcomes, serious adverse events in pregnant people, serious adverse events in infants, and pre-term birth for serious concerns for indirectness due to the difference in the trial dosing interval, compared to the approved dosing interval.
We did this because 55% of the phase 3 trial population and 62% of the phase 2B trial populations did not receive vaccine doses during the approved dosing interval.
There is likely less opportunity for serious adverse events during pregnancy, including preterm birth to occur, when dosing starts at 32 weeks gestation as compared to 24 weeks gestation. And in particular, the risk of preterm birth would likely be lower with dosing starting at 32 weeks than with a dosing window that starts at 24 weeks gestation.
…
Katherine Fleming Dutra, CDC [12:33:05]
In a value survey of pregnant and recently pregnant people conducted from December 2022 and January 2023, 68% of respondents had knowledge of RSV prior to taking the survey, 61% of respondents said they definitely or probably would get an RSV vaccine while pregnant.
And among those who did not respond, that they definitely would get an RSV vaccine while pregnant, safety concerns, lack of RSV knowledge, and concerns about vaccination causing or intensifying RSV infection were the top reasons for not wanting an RSV vaccine during pregnancy.
It’s also important to look at the uptake of other vaccines in pregnancy. We know that in the U.S. coverage for recommended vaccines among pregnant people has decreased during the pandemic and varies by race and ethnicity. Tdap vaccination coverage was 53.5% in the 2020 to 21 season and 45.8% in the 21 to 22 season. Rates of Tdap coverage were higher in white non-Hispanic women than among black non-Hispanic women during the 2020 to 21 and 21 to 22 seasons.
…
Katherine Fleming Dutra, CDC [12:35:43]
Another important consideration for feasibility is simultaneous administration of RSV vaccine with other vaccines in pregnant people. Pregnant people may potentially be eligible to receive RSV, Tdap, COVID 19, and influenza vaccines at the same visit.
There are limited data regarding simultaneous administration, but there was a Pfizer study in healthy non-pregnant women ages, 18 through 49 years, on simultaneous administration of Tdap and Pfizer RSV vaccine that found decreased immune response to pertussis components, meaning that non-inferiority criteria were not met.
However, given the lack of correlates of protection for pertussis, it is unclear how this might impact protection against pertussis from maternal Tdap, when simultaneously administered with RSV vaccine.
Tdap is recommended every pregnancy preferably during the early part of gestational weeks, 27 through 36, which means that Tdap would preferably be given before 32 weeks, an RSV vaccine would be given on at or after 32 weeks. However, in market scan data from 2018 through 2021, about half of captured Tdap doses were given before 32 weeks gestation.
…
Katherine Fleming Dutra, CDC [12:36:57]
Another important consideration is that RSV vaccine is one of two available preventive products for RSV in infants, either RSV vaccination during pregnancy or nirsevimab administration for the infant, after birth, can be used to prevent RSV disease in infants, but the work group felt strongly that both products are not needed for most infants.
The pregnant person and their prenatal care provider will need to make the decision during pregnancy regarding which RSV prevention product to use. Many prenatal care providers may not have time to discuss options for RSV prevention with their patients and prenatal care providers may not feel equipped to discuss nirsevimab as this product will be given to the infant after birth.
…
Katherine Fleming Dutra, CDC [12:37:39]
Regarding the timing of RSV vaccine dosing during the calendar year RSV vaccine dosing could be implemented for pregnant people as a seasonal campaign or year round.
The work group unanimously supported use of a seasonal dosing strategy for maternal RSV vaccine, because this would maximize cost effectiveness and maximize benefits for infants. And it targets RSV vaccine dosing to infants who will be in the first months of life during the RSV season.
And importantly, another product, nirsevimab, is available for infants who were born out of season for whom maternal vaccine protection would have waned by RSV season.
The work group supported seasonal dosing beginning in September and going through January in most of the continental United States based on typical or pre pandemic RSV seasonality. This aligns with implementation of influenza vaccine and thus would simplify implementation for prenatal care providers.
The work group felt that jurisdictions in which RSV seasonality differs from most of the continental United States should have flexibility regarding start and stop of administration of RSV vaccine in pregnant people. And these jurisdictions include Alaska and jurisdictions with tropical climate such as those listed here.
…
Katherine Fleming Dutra, CDC [12:39:24]
The base case is shown in the first bar at about $400,000 per QALY. And if the months of dosing are limited to target dosing to pregnant people whose infants will be in the first months of life during the RSV season, the incremental cost effectiveness ratio or ICER decreases, meaning that the cost effectiveness improves.
And importantly, you can see the ICER for providing doses during September through January, the work group’s preferred dosing timing is $167,000 per QALY.
RSV vaccine may improve RSV outcomes, but it will also increase costs. The base case model showed an ICER of about $400,000 per QALY. And the base case assumed year round dosing of this vaccine and typical RSV seasonality in most of the continental United States.
The work group felt that this vaccine would not be cost effective under the base case conditions. However, cost effectiveness would be improved by using a seasonal dosing strategy, during September through January in most of a continental U.S., thus, as we have discussed already, the work group unanimously supported the use of a seasonal dosing strategy.
…
Katherine Fleming Dutra, CDC [12:41:49]
Regarding insurance coverage of pregnant people by Medicaid and of coverage of vaccines during pregnancy, by federal law, all states provide Medicaid coverage for pregnancy related services, to pregnant women with income levels up to 138% of the federal poverty level.
In 2021, 41% of mothers had Medicaid at the time of birth, making Medicaid the largest payer for maternity care in the United States.
If recommended, ACIP will vote on a Vaccines for Children resolution for this vaccine for pregnant people age less than 19 years, and beginning on October 1, when the Inflation Reduction Act provisions become effective, state Medicaid agencies will be required to recover vaccines and their administration without cost sharing for nearly all full benefit adult beneficiaries covered under traditional Medicaid, if the CDC ACIP recommendations apply.
…
Katherine Fleming Dutra, CDC [12:42:40]
Regarding other insurance coverage, meaning commercial insurance for vaccines during pregnancy, under the Affordable Care Act and its implementing regulations, ACIP recommendations that have been adopted by CDC and are listed on CDC’s immunization schedules generally are required to be covered by group health plans and health insurance issuers without any cost sharing requirements.
…
Katherine Fleming Dutra, CDC [12:46:37]
The work group had extensive discussions regarding a full recommendation versus a shared clinical decision making recommendation.
Most work group members support a full recommendation. They felt the approved dosing interval reduces the potential risk and complication potential risk of and complications from preterm birth. They stressed the importance of clear vaccine recommendations. They noted that providers who will help pregnant people decide which product to receive generally have less familiarity with the data than ACIP does. They expressed that shared clinical decision making recommendations can be confusing, hard to implement for providers, can lead to lower vaccine confidence and uptake, and could potentially influence support for the vaccine in lower and middle income countries where nirsevimab may not be available.
A minority supported a recommendation was shared clinical decision making. They noted that without shared clinical decision making, a full recommendation could result in some providers recommending RSV vaccine during pregnancy, without discussing with pregnant patients that nirsevimab is an option. They cited the potential risk for pre-term birth and neuroinflammatory events and cited that the same vaccine is recommended under shared clinical decision making for adults ages 60 years and older.
It is important to note that ACIP generally makes shared clinical decision making recommendations when individuals may benefit from vaccination, but broad vaccination of people in that group is unlikely to have population level impacts.
And lastly, as we discussed in June, the work group noted that currently there are no data available on the efficacy of the first lifetime dose during subsequent pregnancies, nor the safety of additional doses given in subsequent pregnancies. The work group felt that it was too early to decide whether additional doses should be given in subsequent pregnancies given the lack of data, and additional data are needed to inform whether additional doses and subsequent pregnancies would be indicated and recommendations can be updated in the future.
…
Jefferson Jones, CDC [12:53:29]
The work group felt that for most infants administering both products is not needed. And based on the cost effectiveness analyses presented earlier today, this would not be a reasonable and efficient allocation of resources.
Of note, the documentation of maternal vaccination status may not be available to the infant’s healthcare provider.
Most work group members felt that pregnant people should be aware that both maternal vaccination and nirsevimab are options when deciding whether to be vaccinated. However, healthcare providers of pregnant people may not have the time or feel equipped to discuss nirsevimab when counseling.
The work group felt that in rare situations, flexibility is needed for providers to be able to administer nirsevimab when it is clinically warranted to infants, born to vaccinated mothers.
Examples include conditions in pregnant people resulting in an inadequate immune response to vaccine or decrease in trans placental antibody transfer. Also infants who have undergone cardiopulmonary bypass leading to a loss of maternal antibodies and infants with sufficiently increased risk for severe disease to warrant nirsevimab because of the potential increased benefit.
…
Jefferson Jones, CDC [12:54:51]
So the following are the proposed clinical considerations for the use of the maternal RSV vaccine and nirsevimab.
Either maternal vaccination or use of nirsevimab in the infant is recommended to prevent RSV lower respiratory tract infection. But administration of both products is not needed for most infants.
Healthcare providers of pregnant people should provide information on both products and consider patient preferences when determining whether to vaccinate the pregnant patient or to not vaccinate and rely on administration of nirsevimab to the infant after birth.
…
Jefferson Jones, CDC [12:55:32]
So this slide displays potential information that could be shared with patients on the relative risks and benefits of a maternal RSV vaccine and nirsevimab.
It is important to note that both products are safe and effective in preventing RSV lower respiratory tract infection in infants.
Relative benefits of maternal vaccination includ: a maternal vaccine provides protection immediately after birth when infants are at the highest risk for severe RSV disease, a maternal vaccine may be more resistant to virus mutation compared with monoclonal antibodies, although RSV does not mutate rapidly.
While both products require an injection, use of a maternal vaccine avoids injection of the infant.
Relative risks of maternal RSV vaccination include: maternal vaccine induced protection is reduced if fewer vaccine induced antibodies are produced, for example, if mother’s immunocompromised or could be reduced in transferring from mother to baby. For example, if the infant is born soon after vaccination.
There is a potential risk of pre-term birth, but administration at 32 to 36 weeks reduces this risk.
Relative benefits of nirsevimab include studies of antibody levels suggest that protection from nirsevimab mightt wane more slowly. Administration of nirsevimab can provide antibodies directly, if an infant receives less antibodies from the mother. And since nirsevimab is provided after birth, there are no risk of adverse pregnancy outcomes.
Relative risks of nirsevimab include there is potential limited availability of nirsevimab during the 2023 to 24 RSV season.
…
Georgina Peacock, CDC [01:02:41]
There has been a lot of conversation already about cost of the vaccine.
So the cost of the Pfizer RSV vaccine is $295 a dose, compared to for Tdap approximately $46 to $52.
This cost is lower than the infant nirsevimab cost of $495 for the private sector cost.
Reimbursement and cost recovery challenges have already been identified by providers and practices as an implementation barrier for maternal immunization. And you’ll see that on this slide here, that when looking at the different provider concerns, financial concerns really are the leading barrier to maternal immunization.
…
Georgina Peacock, CDC [01:04:46]
What we’ve heard anecdotally is that plans are starting to let people know that they will start covering nirsevimab when it comes out in the coming weeks.
…
Georgina Peacock, CDC [01:05:14]
As far as supply and availability of maternal RSV vaccine and nirsevimab in this 23-24 RSV season, we don’t anticipate any supply demand mismatches, because the Pfizer maternal RSV vaccine is the same product in use for adults aged over 60 years of age, availability is expected shortly after ACIP recommendations.
Nirsevimab is likely going to be available very soon. And we anticipate this being available as soon as next week, or in early October.
…
Georgina Peacock, CDC [01:06:01]
There are efforts underway to increase the number of birthing hospitals who will be able to administer nirsevimab, particularly under the VFC program.
…
Georgina Peacock, CDC [01:06:14]
One thing to point out is that the increase in complexity of the maternal immunization schedule. And so you’ll see here, um, the different potential recommended vaccines during pregnancy.
So influenza COVID 19 and Tdap P and then, this RSV vaccine and seeing that there are different timings of the vaccines based on season or, and, or gestational age a limited window for RSV administration. And it’s really unclear about the willingness of pregnant people to accept multiple vaccines in pregnancy.
This gives us a little bit more information. And so in a survey of pregnant people 12%, they would accept no vaccines. And if you look at those that would accept either one or two vaccines together, that’s about 49%. This is another piece of information to look at uptake of vaccines among pregnant people. And this has declined as well as we see that disparities persist.
…
Georgina Peacock, CDC [01:08:12]
When we think about pediatric provider roles in immunization decisions, the pediatrician or the pediatric provider recommendation for RSV is really, or sorry, for nirsevimab, is contingent upon knowledge of maternal vaccination status. And we know that this could be challenging if the pediatric provider doesn’t receive the maternal record.
Verbal report of vaccines received during pregnancy may not be reliable. And therefore pediatric providers may need to make decisions on nirsevimab administration without having complete information on what happened during pregnancy.
We also think about the capture of the immunization data. State IIS’s vary in what they capture related to adult immunization. So pregnancy status is not identified in IIS, though there is a potential way to look at the immunization information system data, because you could use adult women less than 60 years of age as a proxy for this RSV vaccine administration.
There is not a way currently to link maternal and infant immunization records in immunization information systems. So it would be— it’s not possible through these systems at this point in time to be able to use that, to forecast whether or not an infant nirsevimab immunization is needed.
There are also in some state policies, there’s not an ability for pediatric providers to review adult records, or records of individuals who are not their patients.
…
Georgina Peacock, CDC [01:10:13]
There are, as there always are in immunization implementation, some communication challenges.
The terms like vaccine for the maternal product versus immunization for the infant product, understanding what the potential risks and benefits are, and helping a pregnant person make an informed decision.
This is something that is going to take time for providers to have those conversations and then discussing financial implications to a patient in a setting of uncertainty related to coverage in this first year of implementation.
…
Georgina Peacock, CDC [01:10:55]
There is a lot of work being done here at CDC. There have been formative research and message testing. So a lot of focus groups and in depth interviews to help inform the ultimate communication activities that will be done for the public.
There have been surveys of parents, of young children, also pregnant and recently pregnant people with that information patient and provider education materials are being developed.
There’s also some partnerships with healthcare provider organizations, as well as those organizations that serve pregnant people and an intention to do social media across all of CDCs platforms.
…
Luis Jodar, Pfizer [01:14:43]
We want to assure the committee that a robust supply of vaccine is already available to providers and ready to be implemented through existing vaccine programs.
The RSV season is already starting, and for the first time, we could have importantly two routinely recommended options for RSV prevention for infants. Pregnant persons will now be able to have an informed discussion with their OB’s and other maternal health providers as they do for all routinely recommended maternal vaccines and make an informed decision on which option is best for them and their baby.
Finally, I would like to emphasize that the RSV vaccine will be a lower cost option, and overall could result in lower budget impact for the U.S. healthcare system.
…
Sarah Long, ACIP [01:24:05]
And as far as you consider our very restricted suggestions for the use of nirsevimab after the receipt of appropriately timed vaccine, in that you consider that these are both antibody paint, and that the antibody paint will wear off. And it doesn’t change the epidemiology of RSV disease. And its goal is not to prevent RSV infections in every individual.
It can only reduce by a certain degree, the morbid consequences of RSV disease. So people have already— pediatricians and others have already been concerned about our cut points for nirsevimab and our cut points for this. And they are based on data.
And because this is not a vaccine that will change the epidemiology, prevent herd, prevent long term protection, we have to have those to make them both cost acceptable because these are extraordinarily, probably unreasonably priced products.
And we would say, bring on competition to bring these down.
…
Keipp Talbot, ACIP [01:26:01]
I think this might be the most complicated vaccine recommendation for young adults that we’ve had in a long time. And I worry about the complication of the time period.
I know we give flu and COVID during that season, but we give it to everybody regardless of where they are in their pregnancy. So there’s a lot less of a needle with those two vaccines.
I also am a little bit worried, in the adult world, if you get the same vaccine twice, you pay for the second vaccine. So if a mother has not gotten her— she’s gotten her RSV vaccine, but is confused because she’s gotten four vaccines or two vaccines or three vaccines, and the pediatrician’s kind of left in this position to give the child the antibody, someone’s going to have to pay, because that’s double dipping since we’re only recommending one or the other.
I think it’s really interesting that mothers don’t want four shots. They want less than that?
So I guess I’m asking what’s the benefit of this vaccine, if we’re gonna give every child antibody, why do we need to recommend it at all? So I’m hoping the work group can help me work through that struggle.
…
Katherine Poehling, ACIP [01:28:18]
I would like to respond to Dr. Talbot. And in speaking to parents who have recently given birth, there are some that would prefer to take a vaccine rather than have their child get a shot.
And then there’s also all kinds of cases that I’ve had recently, including one where the father of the child had a significant bleeding disorder. And so they didn’t want the child to have any sticks for any reasons, because we didn’t know if that child was going to have a bleeding disorder.
So there’s going to be multiple cases like that.
But you are absolutely correct. There is a lot of complexity, and a lot of clearly documenting the information. So everybody knows what has and hasn’t been received is going to be extraordinarily important. And it builds on what you’ve said in last meetings, that having an immunization registry for all is desperately needed.
…
Georgina Peacock, CDC [01:31:49]
There’s very limited availability of funds through the 317 program.
Those funds haven’t decreased in amount. However, there are more vaccines that are potentially could be paid for, for uninsured adults, through our 317 funds. And so really there’s very limited availability, in the big scheme of things, to be able to pay for additional vaccines through this limited pot of 317.
And I guess just for context, the 317, basically, we give a portion of funds to all of our immunization awardees so that they can purchase some vaccine. Typically this is used for uninsured adults. Sometimes it fills in some gaps related to children, and then it’s also used for outbreak funds.
So it sort of— and so it’s a fairly limited amount of money.
…
Pablo Sanchez, ACIP [01:36:47]
I actually was one of the ones in favor of the shared decision making, because I think there are two options that need to be discussed with the pregnant woman and with— because it’s not just the vaccine at 32 to 36 weeks, but she needs to be told also that the other option is nirsevimab.
And that, I can imagine as a pediatrician taking care of a baby who I then tell the mother that this baby cannot get nirsevimab because she had chosen to receive the RSVpreF RSV vaccine. And so I think that that discussion, irrespective of what is easy or not easy, and what the obstetrician and healthcare provider for the pregnant woman decides, I think that discussion must be had, and it it’s been stated already, but I think that that is important.
And so when I think that there’s a variety of options to be discussed, I think shared decision making is the way that I would prefer.
…
Grace Lee, ACIP [01:38:19]
In my opinion, every recommendation should really be a shared decision, similar to all medical care that we provide. I think, the distinction about the recommendation is not whether or not the process occurs. It’s really more about sort of more of a universal recommendation versus more of a selective recommendation.
So I don’t think that a full recommendation means that this discussion shouldn’t happen. In fact, it should with every pregnant person, to make sure that they’re aware of the options. That’s my opinion about it. And I don’t think shared clinical decision making changes that. I think it just restricts the access for certain patients.
…
Lynn Bahta, ACIP [01:39:48]
The feasibility of this I think is really challenging.
As I know from the colleagues in my own health department, are struggling with how to implement the nirsevimab and how to reconcile that if the preF is also recommended. How to coordinate that.
And I also want to emphasize something that Dr Peacock mentioned, and that’s related to the 317 funds. They are incredibly restricted, but not only that, programs are implementing the seniors RSV, which is also a very costly vaccine, and will be in very limited supply.
So there will be a lot of competition, and probably very little supply or availability of that vaccine for either audience. And, so I think that’s an ongoing issue that we need to keep thinking about.
…
Katherine Poehling, ACIP [01:46:36]
We in North Carolina have one insurance company that has agreed to pay for nirsevimab in the outpatient setting. We’re still waiting on the inpatient setting. So that is just where people are.
And I do— I am worried about the cost and who’s going to cover it. So I do think this is a very important option. And so, I would like to make a motion to accept the voting language as it is written.
…
Pablo Sanchez, ACIP [01:47:25]
Just thinking about what Dr. Loehr had commented, which is— which I agree it is what we have discussed for the clinical considerations.
But as I think about it, actually, if we diagnosed severe congenital heart disease, for instance, or some other malformation that may be beneficial to really provide more substantial protection, actually, that infant is likely to stay in the NICU or the cardiovascular, the CT ICU, for a prolonged period of time, and actually thinking about it, nirsevimab would not be given until discharge.
And although we try to prevent RSV infection in these units, it does occur. So I’m just thinking that actually some of those babies, may actually benefit if they have maternal antibody, at least through the time of discharge.
So, and in those infants, we have recommended, or that nirsevimab be given, and that even irrespective of whether the mother got the vaccine, so I’m just throwing a different angle to that.
So I think that it would be best kept in the clinical consideration.
…
Brenna Hughes, ACOG [01:50:59]
Related to the shared clinical decision making comments, that in fact obstetricians are quite experienced and routinely perform counseling for all patients who receive vaccines, and this would be no different.
And would agree with Dr. Long’s assertion that for that reason, this does not rise to the level of a shared decision making policy discussion and would support the full recommendation on behalf of ACOG.
…
Jamie Loehr, ACIP [02:04:49]
I actually want sort of go on record that I still believe that if a child is going to get nirsevimab, that is better. I think it’s better because we seem to have evidence that it’s better efficacy. It’s definitely more cost effective.
And so I don’t really want it to be an equal representation. I recognize we’re not gonna make a preference. And I recognize that we need a lot more data over the next couple of years to see in the long run, which is better. I doubt we will ever get head to head information, but I don’t want it to sort of be that, you can get this one or you the kid can get the vaccine, the nirsevimab.
I sort of, if I’m presenting it to a pregnant woman, I’m going to say, if you want to give your kid nirsevimab, that’s what I recommend. And if you don’t, then this is another option. That’s just a small nuance on what Dr. Long said.
With regard to Dr. Sanchez, I would go back to what the work group said. I see shared clinical decision making when you have a good product that has some drawbacks that the person should really know about.
And so I could see where you might say nirsevimab is better. And so that’s a drawback, but really the classic one for me is where we have RSV for adults. And I’m spending a lot of time telling people about this potential neuro complication from the vaccine.
So I recommend the vaccine, but there’s this problem, possible problem with it. That’s where I would use shared clinical decision making.
So that’s why I don’t think it quite rises to that level.
…
Pablo Sanchez, ACIP [02:16:27]
We all have personal preferences. And we look at the data, and we look at the efficacy of the trial of the— one of the trial, of the two trials of the preF vaccine and also of niresvimab, and unfortunately the end points were different. So we can’t even compare the actual, head to head in many instances, in terms of primary outcome.
But I think we all have preferences for one or the other. And I think— and I have to come back to the point that what we’re doing is voting on this vaccine, not on how it’s gonna compare to nirsevimab, because ultimately we need that to be studied.
…
Brenna Hughes, ACOG [02:17:19]
One is that it is absolutely routine for us to, as obstetricians, and to collaborate with our pediatric colleagues to review maternal charts. It is done every day regarding testing like hepatitis B testing, those are results are always communicated. And so while we recognize that there is some complexity to ensuring that the charts are complete, related to receipt of vaccine, it’s quite doable also acknowledging the fact that this is fairly complex.
And we at ACOG along with our CDC colleagues, the Society for Maternal Fetal Medicine, plan to partner with other entities like Mother to Baby, American Academy of Pediatrics, AAFP, and ACNM to ensure that there is a solid implementation strategy to assure that these challenges are met.
…
Katherine Fleming Dutra, CDC [02:20:18]
We wanna make it very clear that again it’s important for pregnant people, when they are making the decision during pregnancy, should this vaccine be recommended, whether they would receive the RSV vaccine or nirsevimab, that that conversation happens.
And it would not be, I just want to clarify that. So if a pregnant person presents, there are 32 to 36 weeks during September through January, that conversation should happen, whether they would prefer to receive the RSV vaccine, should it be recommended or nirsevimab.
It’s not that one would be preferred at a certain timing.
…
Grace Lee, ACIP [02:48:27]
If I counted correctly, I think it’s 11 yes’s and 1 no.
Melinda Wharton, CDC [02:48:31]
I counted the same way you did Dr. Lee. So the motion passes.
…
Grace Lee, ACIP [02:50:22]
So Dr. Wharton, I have 11 yes’s and 1 no. And the VFC vote passes.
…
Beth Bell, ACIP [02:51:58]
I just wanted to take advantage of my gray-haired status here and reflect for a moment on this issue of complicated recommendations where implementation is unclear, difficult, not that the implementation is going to be difficult, there are a lot of challenges.
And I will say to your point earlier, Dr. Lee, that in looking back over decades, hepatitis B vaccination, being an obvious one that comes to mind, I think these sorts of recommendations that provide an opportunity for innovation that provide availability of different options.
Oftentimes, while at the beginning might be extremely bumpy, oftentimes do drive improvements over the longer term. And I think that this is another example of that.
It allows perhaps for improvements in physician education, patient decision making, communication between the obstetrical world and the pediatric world, addressing disparities.
So even though we as ACIP members at this moment in time may feel like, ‘whoa, this is really complicated, and it’s gonna be very difficult to implement.’
I think in the longer term, as I say, it provides an opportunity and some new options that I think will improve children’s health in the longer term.
…
Jeanne Santoli, CDC [03:05:34]
Traditionally, the schedules are published in February, but the publication process starts in October with the ACIP vote.
In November and December, professional organizations approve the schedule. And in December and January, we draft and enter into CDC clearance, MMWR reports and an Annals of Internal Medicine report.
And then in February, the schedules are published along with the accompanying MMWR notice to readers and Annals of Internal Medicine report.
…
Jeanne Santoli, CDC [03:06:13]
The timeliness of schedule publication has several important implications.
First, some insurers link vaccine reimbursement to the vaccine being listed on the immunization schedule.
Second, the ability of certain healthcare providers to administer immunizations is also related to the schedule. For example, some states link pharmacist immunization authority to the schedule.
And lastly, healthcare provider knowledge and practices are related to the immunization schedule. For example, if a healthcare provider is referring to a schedule that several months old, they may not be aware of the most recent ACIP recommendations.
…
Jeanne Santoli, CDC [00:07:04]
The Affordable Care Act addresses immunization coverage, and it’s interpreted by CMS.
According to the Affordable Care Act, insurers must provide coverage for, and must not impose cost sharing restrictions for immunizations that have a routine recommendation, and that are listed on the immunization schedule of the Centers for Disease Control and Prevention.
Of note, the Affordable Care Act does not specify the layout of the immunization schedule. So legally, CDC has discretion regarding the design of the immunization schedules, and it’s the entire document that constitutes the schedule, not just the graphic bars or the tables of the schedule.
…
Jeanne Santoli, CDC [03:07:57]
We are looking at a three-pronged approach to address schedule timeliness.
Our immediate strategy consists of the addition of addenda, to help bring the schedule up to date.
Our short term strategy involves publication of the entirety of the schedule shortly after the October ACIP vote.
And our longer term strategy is to consider sustainable approaches to ensure the schedule remains dynamic and responsive, and we will engage our partners in the planning process.
…
Jeanne Santoli, CDC [03:08:36]
So regarding the addition of the addenda to, to the 2023 immunization schedules.
The addenda will contain ACIP recommendations that occurred after the 2023 schedule was published. We plan to release the 2023 immunization schedules with the addenda next week.
And with this addition, all ACIP recommendations will formally be part of the CDC immunization schedules.
…
Jason Goldman, ACP [03:12:23]
It is imperative that the schedule will be updated, approved, and published as quickly as possible to avoid unnecessary delays in implementation.
The college greatly appreciates the willingness of the CDC to expedite this process. The lack of insurance coverage creates unnecessary barriers to access to care, and further exacerbates healthcare disparities as uninsured and underinsured patients will not have access to these vaccines.
…
Sean O’Leary, AAP [03:14:15]
The publication of official CDC recommendations is an essential step in this process.
As an example, considered the PCV20 vaccine, the pneumococcal conjugate vaccine, which was recommended by the ACIP at its June meeting.
AAP members have recently reported that some VFC programs are providing only PCV20 and that some vaccine buying groups are directing people to use this vaccine over other pneumococcal vaccines.
However, this is problematic because a lack of formal recommendations in an updated immunization schedule or publication in MMWR is leading to payment denials for PCV20, as well as delays in Tricare coverage for children and military families.
Timely updates to the immunization schedule would provide pediatricians with an authoritative source for the latest immunization recommendations, which is invaluable at the point of care to maximize every opportunity to vaccinate.
Merck statement on commercialization of Lagevrio
- Source: statement emailed by a Merck spokesperson
- Date: received September 22, 2023
We continue to have ongoing discussions with the FDA about the data package needed to support the initial NDA for LAGEVRIO (molnupiravir). In the meantime, we are working closely with the U.S. government to ensure patients have continuing access to LAGEVRIO.
We are working towards transition to commercial market supply later this year. Because this is based on multiple factors, this timing may be subject to change.
FDA official on updated COVID vaccines
- Source: video posted by Food and Drug Administration
- Date: published September 21, 2023
Question [00:06:11]
Can you also talk to whether or not it’s recommended to coadminister this vaccine with other vaccines, such as the flu vaccine?
Peter Marks, FDA [00:06:19]
Right. So this is a matter of preference, but as was discussed at the ACIP yesterday, perfectly fine to give this vaccine with other vaccines and many people will get it with the influenza vaccine. There’s no reason why they can’t be administered together.
I have to be an honest person and say that some people are saying, ‘well, could I get RSV, COVID, and the flu vaccine on the same day?’
Yes, indeed, you could. But honestly, I might not, just because each of them can potentially make one a little a little fatigued or have a little bit of a fever, and I might just want to space them out a little bit, but if you had to drive a lot of miles to get the vaccines, and that it might not be unreasonable to get all three of them at once.
…
Peter Marks, FDA [00:10:03]
I think the the issue that may come up as a discussion later on this year, but not right now, is whether older people would potentially need a second vaccine. That’s not at this time, that’s not under consideration right now.
The recommendation is older people, those with disabilities, including people without disabilities, such as pregnant people, also, that they go ahead and get vaccinated.
…
Peter Marks, FDA [00:12:48]
If you want to get them separately, you know, in general, this is just guidance that– general guidance. It’s not a– this is not a must.
But oftentimes we suggest, if you want to minimize the chance of interactions, and minimize confusing side effects from one with another, you wait about two weeks between the vaccines.
To be perfectly honest, I’ll tell you if it, what I’m thinking of, I’m probably gonna go out this Friday, Saturday, get my COVID vaccine. I usually get my influenza vaccine around October 1st. The flu vaccine doesn’t last tremendously– it has a little bit of a shorter life than we might like, in some ways it’s a little like the COVID vaccines.
And so that’s how I would go about it, but with about a two week separation, but it’s not– just know, that’s just general guidance, not anything that’s a must or so, so this is a discretionary thing.
…
Peter Marks, FDA [00:14:52]
So we’re very lucky.
One of the things I’ve learned from getting towards the end of the third full year of pandemic response, it feels like 20 years because each year feels like a dog year, seven years per year, but one of the things we’ve learned is that some of what we have to deal with is just luck. And we actually were lucky.
It turned out that XBB.1.5, which is a BA.2 descendant, and the other variants that have emerged are also BA.2 descendants. And so, when we look at the ability of the current vaccine to actually neutralize the circulating EG.5 variant, which is, I believe right now, the most common variant, as well as even the BA.2.86 variant, which is present in small amounts, but people were concerned about because of all of the mutations, it actually does a really good job on both of them, in fact, almost as well or better than the XBB.1.5.
So, I think we’re very lucky that we have a vaccine that’s a good match. And that’s one of the reasons why I wouldn’t– when you have a good– it’s like having a bird in the hand. I have a bird in the hand, good match, a lot of COVID around, great time to go get vaccinated, because I think the idea here is that risk reduction at this point is a good thing, especially because all of us, myself included, have been less probably less fastidious in our COVID precautions.
…
Question [00:18:31]
There’s another question in here about the anticipated timeframe for the vaccines that were authorized under EUA. So the updated COVID vaccine for those 12 years of age and younger to be fully approved.
Peter Marks, FDA [00:18:47]
So people have been interested in when that will happen. What were really just– what happened was those studies started later. And so in order to get to a full approval, we like to see either 6 or 12 months of safety follow up. So these submissions for the licenses came in later.
We would expect that sometime, I, again, can’t give you an exact date, but sometime by early 2024, we’ll see those full approvals across all the age ranges, because by that time we’re hoping to roll up and no longer have EUAs and have licensed vaccines all around.
Question [00:19:24]
And can you talk a little bit about whether or not, if there’s any sort of, you’ve explained before the difference between an EUA and a fully authorized vaccine, can you describe sort of that difference in months and how you get the data for an authorized vaccine?
Peter Marks, FDA [00:19:43]
So the authorized– in this particular case, the difference between the emergency authorized vaccines for the children under 12 and the licensed vaccines for those over 12, the effectiveness data in these cases is very similar. They met the effectiveness standard that we would use for licensing of vaccine.
It’s just a matter of the quantity of time for safety follow up, which we required at least a median of two months for kids. Now, we actually have significantly more than that, that we’ve reviewed, but it’s a matter of having the manufacturers actually submit that in an application, doing the inspections of the facilities that are making these different formulations, and issuing a license. And those will just take a couple more months to get there.
But I feel confident in telling people that those EUA vaccines are every bit as safe, effective, and trusted in terms of their quality as the licensed vaccines.
…
Peter Marks, FDA [00:23:52]
I kind of alluded to this before.
Right now, there’s only one dose expected for people 65 and up, but I think as we see, we are constantly evaluating the circulation of COVID 19, the number of cases, and how things are going. And I think if we saw that it appeared that people might benefit in a few months from an additional dose, we would probably work with our CDC colleagues to issue a recommendation at that time.
But right now we are just talking about a single recommendation, a single dose recommendation.
…
Peter Marks, FDA [00:25:14]
Thank you so much because I’d love to explain that.
We’ve decided not to use it. You noticed that I’ve been trained not to use that word, and I’m not going to say it. Dale will say it for me.
But instead we’re calling it an annual update for the vaccine. We want people to understand that this is an annual update. There’s no reason– it’s the annual vaccine, and I think, honestly, we– I feel like we want a very big tent. People who have decided they didn’t want an a COVID vaccine before, because they were nervous about the new mRNA technology or this and that, they don’t have to feel like they’re gonna have to be singled out or anything. Everyone just needs one dose of the annual update to be up to date if you’re an adult, or if you’re anyone five years of age or so, so I think this should hopefully make it a little easier.
Again, we want to remove as many barriers as we can to help people get vaccinated.
…
Question [00:26:32]
Are there any updates on the approval of Novavax?
Peter Marks, FDA [00:26:36]
Happy to tell you that it– we hope to see that in the next few weeks. We are working diligently.
September 21, 2023
HHS vaccines advisory committee meeting updates from liaisons
- Source: webcast of National Vaccines Advisory Committee by the Department of Health and Human Services
- Date: broadcasted September 21, 2023
Manisha Patel, CDC [01:13:51]
I serve as the chief medical officer for the National Center for Immunization and Respiratory Diseases at CDC, and we have a couple of updates for the committee.
First is that we did welcome a new leadership team last month. Dr. Demetre Daskalakis is serving as the acting center director for NCIRD. And Dr. Amanda Cohn is serving as the acting principal deputy director, and Dr. David Wentworth is now serving as the permanent director for our newly stood up Coronavirus and Other Respiratory Diseases division.
And then the second update, as many of you are aware, CDC is preparing for the fall and winter respiratory season. And this is a priority for our agency. And we have transitioned our center-led COVID-19 activation to a center-led respiratory virus response activation, to include flu and RSV in our activities.
And three of our major goals, within that response, is number one to conduct rapid and robust surveillance, including detection of emerging variants. Second is timely communication with partners, such as yourselves, providers and the public. And third is adoption of our new and updated vaccine recommendations, and specifically, COVID 19 and flu vaccines, which are now recommended for everyone six months and older.
And we have new immunization products for RSV. The first is nirsevimab, which is a long acting monoclonal antibody recommended for all infants less than 8 months. And then a smaller group of infants 8 to 19 months who are at higher risk for RSV are recommended to get nirsevimab in their second RSV season.
And then the second product is RSV vaccines for adult 60 and older, under shared clinical decision making. And then tomorrow there will be an ACIP vote for RSV, use of RSV vaccines, in pregnant people. And, look forward to talking more about this tomorrow afternoon.
…
Rebecca Coyle, AIRA [01:29:44]
We are also very excited to have RSV products in the arsenal.
One of the things I just wanted to note, I think from the system side, there’s always, clearly there’s the vaccines that are usually entered very quickly and easily, and that seems to be the case as well, as of now, we know that a majority of IIS can accept RSV vaccines into the IIS. So that’s very exciting.
There is one exception to that, that I just want to note, and that’s related to nirsevimab, because this is not a traditional vaccine product and doesn’t follow the traditional vaccine product codes, it’s not sitting in a system vaccine code set. That means that, for the 80% plus of data, it originates outside of the IIS, meaning it’s coming from some other data source like VA or a pharmacy system or EHR. It’s not being directly keyed into the IIS.
That means that those systems also have to make updates to their systems to trigger that message to go from that system to the IIS. So there is a difference there in that most systems that for a new vaccine, it just automatically triggers and get sent to the IIS So there’s a difference there.
I think the great thing to note is that again, with much like RSV vaccines, the monoclonal antibody product is also able to be accepted by IIS at this point. So we’re really thrilled to see that happening, but it is important to note like, if it never makes it to the IIS, we won’t ever know, because it relies on our partners out there.
Continuing along that path, I just wanted to note that we are continuing to support the Bridge Access Program, the codes are out there, we’re super excited to see that roll out.
…
Michel Rothholz, APhA [01:33:08]
What I want to spend my time really talking about this point is that, as pharmacies are entering the heavy fall vaccination season, implementation is challenging right now. And I think something that NVAC should look at in a future discussion is the process of implementation. So while we’re getting the recommendations for vaccines coming out, and you heard even Rebecca talk about some things with IIS, I think we should need to take a look at the process for implementation and how do we help get the systems in place?
Because now with social media, the public is aware of these things, as soon as ACIP and the director make their recommendation, they’re coming into the practices, and asking about and asking for those vaccines, but the systems aren’t ready to go yet.
And so we’re seeing that now with the new COVID vaccine, where we’ve got payers who are still in the old system, so when a provider who does happen to have vaccine, that’s another issue that we’ve got right now, is a lot of providers don’t have the vaccine yet, but are getting asked questions about it, but there, when they go to bill for that, it’s still under the old system of where the government provided the vaccine, and not the commercial system, where now the insurance plans have to pay for it.
So that creates a barrier when patients are ready to get vaccinated, the system’s not able to handle it because providers can’t risk losing that amount of money from the system.
So I think we need to look at what’s the timeline for when recommendations are issued to the time when it’s ready for implementation in the market, and may need to look at looking at some recommendations there for giving a little buffer zone for that to occur.
But pharmacies are ready when they’ve got the vaccine, they are handling and talking about co-administration, and we’ve given them resources and encouragement about the co-administration. And so we’re looking forward to a good vaccination season and being productive, working with our partners in the immunization neighborhood.
Alaska’s state health spokesperson on novel influenza variant strains
- Source: email from Alex Huseman of Alaska Department of Health
- Date: received September 20, 2023
The Alaska State Virology Laboratory has not reported out any novel influenza variant strains. All detected influenza viruses have been commonly circulating strains of influenza.
HHS secretary at press conference on COVID vaccines
- Source: recording provided by a spokesperson for the Department of Health and Human Services
- Date: received September 20, 2023
Xavier Becerra, HHS [00:17:52]
There have been some reports, we’ve heard them as well, from people saying, ‘Hey, I’ve got insurance, but I went to go get my vaccine, and I was told I had to pay.’
No, that’s not correct. If you are told that you must pay and you are insured, then please make sure you’re talking to your insurance company, because you should be covered by law, if you are insured, you are covered for COVID. If you are on Medicare, you are covered. If you are on Medicaid, you are covered. And if you don’t have insurance, through this Bridge Access Program, you are covered.
And so make sure that you know the facts, talk to your insurance plan, if they’re looking to charge you, talk to your pharmacist, because sometimes they can clear up what’s going on.
We’ve heard these stories and we’re working with. We’ve contacted the insurers, we’ve contacted the pharmacists, and we’re working with them to make sure everyone understands how this works.
You should not have to pay out of pocket if you are insured. So please, make sure you’re working with your insurance provider or perhaps the pharmacist, or if you need to call us at Health and Human Services, and we’ll try to make sure we get it all straightened out.
…
Xavier Becerra, HHS [00:23:16]
We’ve been working with the insurers for months, with the pharmacists for months, we had to reach contracts with the various stakeholders. So everyone’s known, but sometimes whether it’s a computer glitch or maybe something else, something could get in the way.
My sense is that these are glitches that will be addressed pretty quickly, but if not, please know, first and foremost, you should not have to put money out of pocket to get the COVID vaccine. Two, if you are told that, then make sure you’re getting some names because we’ll try to, we’re all going to be trying to follow up.
I’m sure CVS will do everything it can to make sure that it’s following up to make sure its pharmacists know how it works. And I’m sure that all those insurers, that are making sure that their own members are safe, are going to do what they can to make sure it’s clear.
…
Jay McMichael, CNN [00:22:20]
We’re also hearing that shots for children are taking longer to be available. Do you know why that is? And when can families expect to get their kids vaccinated?
Xavier Becerra, HHS [00:22:28]
So, shots for children– the COVID vaccine is available to anyone six months of age or older.
And so if it’s available, it’s available for your children as well. You may be talking about flu, RSV, or perhaps the flu, but the flu is also very much available. So we’d have to follow up with you.
There is no reason why a child should not be able to get the COVID vaccine if adults are getting it. And we could check to follow up, to see if there’s some issues with the RSV vaccine, but the flu vaccine I’m pretty sure is available to kids as well.
September 20, 2023
ASPR interview about COVID-19 tests announcement
- Source: Zoom interview with Dawn O’Connell of the Administration for Strategic Preparedness and Response
- Date: interviewed on September 20, 2023
Dawn O’Connell, ASPR [00:01:11]
These are tests that we have stockpiled and we started stockpiling tests after the Omicron surge, when we were seeing how hard it was initially for people to find over the counter tests.
So we’ve been building the stockpile and we want to make them available. We know, as we’re heading into the fall and winter, we’re likely, if past is prologue, to see an increase in cases as people move indoors and begin interacting in smaller groups. So we want to folks to continue to protect themselves and to have access to these free COVID tests as they head into the holidays.
We know a lot of folks are gonna see their grandmas and potentially vulnerable populations, elderly, young kids. And this is just one of the tools we continue to want to make available to folks as we head into the fall and winter.
…
Dawn O’Connell, ASPR [00:02:11]
We really think the holidays are one of the driving factors. It’s important that folks, as they begin to gather and start to gather with their family and friends, as they plan their trips, have access to tests. So that’s really been the driving factor.
We have been looking at what we’ve seen before in the increase in cases. We think being able to make tests available is just an important tool that we have and can make available.
We’ve had these stockpiled. We’d rather folks have these tests in their medicine cabinets that they can use now, than sitting in a stockpile somewhere. So we really think it’s just been an important tool, and we made an active decision to make it available now as we head into the fall and winter respiratory season.
…
Dawn O’Connell, ASPR [00:03:23]
We landed on four as a reasonable number. We want to check demand to see how many folks take us up on these and make sure that we have enough and can calibrate that appropriately across the many weeks between now and the holidays, between now and the end of the year.
So we’ll start with four, of course. We reserve the right to up that if we need to, if we were to see a surge different than what we’ve been seeing before, or if a new variant came along and we needed access to tests quicker. The wonderful thing about having a stockpile is we can use it for such cases.
…
Dawn O’Connell, ASPR [00:04:15]
So this captures two really important lessons that we learned in the COVID pandemic.
The first one, which we all saw in March 2020, when everyone needed the same PPE and medical supplies, and no one could find them, and they were all being manufactured somewhere else, we saw what it felt like to have that supply chain pinched when our frontline health responders were wearing trash bags for gowns because they couldn’t get their hands on PPE. We learned that lesson early, and we’ve been working against it since then to make sure that we have the domestically manufactured access to the critical supplies that we need.
Diagnostics of course are one of the most important, critical supplies at the beginning or throughout any outbreak, you need to know who has it, who doesn’t have it, who’s safe, who needs to be treated, tests are important. So having the manufactured here in the United States, really an important lesson that we’ve learned.
The other has the added advantage of course of good jobs and being able to keep high skilled workers here in the United States.
Beyond that, we also learned the lesson when we experienced the Omicron surge, as we were coming out of Delta, heading into Omicron, over the counter tests were just become coming online people and everybody wanted them.
You know, you couldn’t get people to go for those PCR tests anymore at the drug stores. They wanted to know and rightfully so, you want to know standing in your kitchen, whether you have it or not. The convenience of that, the instant ability to read, to know where, whether you’re infected is really important. So we saw this huge demand for over the counter tests.
And then Omicron hit, and we couldn’t keep up with the demand. So we were unable to meet the demand. You remember, people were waiting in line long lines for tests, whatever they could find.
And as we rounded the corner and were able to ramp, it takes about six to eight weeks for manufacturers to ramp up, and they had all ramped down from the early days, they were ramping down because vaccines had come online. People at that point prior to Delta thought vaccines would prevent infection. And that tests wouldn’t be as necessary. We didn’t need as many tests. That turned out to be wrong and we needed to ramp back up, but it took six to eight weeks to really ramp up.
…
Dawn O’Connell, ASPR [00:06:58]
So with these contracts, we’re really excited of the 600 million, they’re going to 12 domestic manufacturers. We talked about why that’s important, but they also are requiring a sort of warm base manufacturing, for the duration of the contract.
And the way we’ve done this is we’ve ordered 200 million tests and we will put those 200 million tests in our stockpile to be deployed, how we need them, against whatever surge or increase in cases we see next.
But most importantly, the lines will keep running. They will not throttle down. They will continue to run tests as we pull them off the line, and should the demand, should we hit a surge and demand for retail pharmacies exceed what the manufacturers are able to provide, we want the tests that we are currently manufacturing to go to them first.
We are giving manufacturers permission to sell their tests to the retailers so they can get on pharmacy shelves in neighborhoods and be available as quickly as possible.
We will then take the tests when demand diminishes. We want them to continue to manufacture tests. We will take those tests and pull them into the stockpile. And this is a way to keep things warm, so we will always be able to ramp up and have enough when needed and then have a stockpile to bridge the gap.
…
Dawn O’Connell, ASPR [00:09:08]
So we opened this to all the domestic manufacturers. We sent out the RFI and encouraged anyone who was interested to apply.
And then, we negotiated the terms based on their capacity, based on what we thought they’d be able to maintain, based on their willingness to maintain. And so all of those factors went into thow these contracts were negotiated. We’re super proud of the 12 that have emerged.
Have really appreciated working with all the manufacturers and all of them had the opportunity to apply for this funding.
…
Dawn O’Connell, ASPR [00:10:00]
We’re going to continue to watch the epidemiology and see what’s out there.
We’re getting to a point where the vaccines are now seasonal. We’re starting to see some repetition. I mean, COVID’s been anything but predictable, but we’re starting to see some patterns that we’re observing and taking into account as we think about the tools the American people need.
So we’ll continue to do that. But again, one of the really important things about the investments we’re making now is that we can pivot, if we have the capacity to produce these tests, we’ll be able to pivot to something, in a place where it may be needed, if it looks like COVID is leveling off. I’m not saying it is, so I want to be clear, but we’ll continue to watch the epi, continue to see what we need in the COVID space, and then, if we needed to pivot, this provides a little bit of flexibility to do that.
FDA advisory meeting on artificial womb development
- Source: webcast by Food and Drug Administration of the Pediatric Advisory Committee
- Date: broadcasted on September 19, 2023
Kalkidan Molla, FDA [09:36:01]
Preterm birth is a significant public health issue in the U.S.
Infants born premature, defined as less than 37 weeks gestational age, represented 10% of all live births in 2020, but accounted for 65% of deaths in infants less than 12 months of age.
The disproportionate contribution to infant mortality is more striking in the most premature infants, where 40% of all infant deaths occurred in extremely preterm infants born less than 28 weeks gestational age, although these infants represented only 0.6% of all live persons.
Among survivors of extreme prematurity, morbidity rates are high in infants treated with the current standard of care. Artificial womb technology devices are intended to treat extremely premature infants, or EPIs, after 22 weeks gestational age, by providing a bridge from extreme preterm birth to later gestation within a physiologic environment that mimics the womb.
…
Elizabeth Durmowicz, FDA [09:46:43]
We need data from clinical trials and children to understand if medical products are safe and effective in children for their intended use. We need these data to protect children from exposure to medical products that may be unsafe or ineffective in children or in a subpopulation of children.
However, we recognize that children are a vulnerable population who cannot consent for themselves, and therefore are afforded additional safeguards when participating in clinical investigations. Safeguards for children are considered essential requirements for the enrollment of children in clinical trials to support medical product development.
With the understanding that we need to conduct research in children, but we must do so in a way that protects this vulnerable population, FDA promulgated regulations governing the enrollment of children in clinical trials that embrace fundamental ethical principles.
An important principle is related to necessity. This principle holds that children should only be enrolled in a clinical trial if the scientific or public health objectives are important to the health and welfare of children and cannot be met through enrolling subjects who can consent personally.
Another principle is about limitations of risks. Specifically, if a trial does not offer the prospect or direct benefit to the individually enrolled child in the trial, the risk to which the child may be exposed must be low for children. There is a limit to the risk that knowledge alone can justify and risks in a trial should be minimized.
Also, children should not be placed at a disadvantage by being enrolled in a clinical trial, either through exposure to excessive risks or by failing to get necessary healthcare or interventions. In addition, children should have a suitable proxy to provide permission or informed consent for them to enroll in a clinical trial.
…
An Massaro, FDA [10:03:10]
It is important to distinguish between the benefit risk assessment that occurs later in the device development life cycle, where approval of a pre-marketing application would require support that the benefits of the device outweigh any associated risk to patients.
This assessment is supported by data that is generated during clinical development of the device.
In contrast, when we are thinking about benefit versus risk to determine whether it’s ethically permissible to proceed with a first in human trial of AWT device, we need to make an assessment of the prospect of clinical benefits and potential device related risks. And we need to make sure that this assessment is judged to be as favorable as known outcomes with standard of care in the neonatal intensive care unit.
In order to make this assessment, we need to review the outcomes we are achieving currently in the proposed patient population, which in the case of the extremely pre-term infant is variable by each completed week of gestation, as well as by the institution where care is received.
We will hear more about this from Dr. Hans later today.
We also need to understand the available data to support prospect of benefit and safety of the investigational device. While data from animal models and relevant clinical experience may help inform this assessment, we recognize that there will always be some unknowns that will need to be accepted as part of the transition to initial clinical use.
The most challenging question is to answer how much unknown is acceptable.
…
An Massaro, FDA [10:10:42]
Returning to the concept of conducting a benefit risk assessment.
We need to consider both whether there is support for prospect of direct benefit and adequate safety and mitigation of residual risk.
With regards to benefit, we will look to animal models to provide data, to support that the intended effect of the device can be achieved. That is organ growth and maturation are supported while potentially reducing at least some of the atrogenic insults that may contribute to adverse outcomes.
With regards to risk. We will again rely on animal models to help inform risk, but note that as we will soon hear from Dr. Zan, differences between species may limit translation of safety. And we will also need to look where possible at relevant clinical experience to help fill gaps.
As I mentioned previously, even with the most comprehensive non-clinical program to develop an investigational AWT device, we expect that there will be unknowns at the time of initiating a first in human trial of such a highly innovative therapy.
We will need to weigh the totality of the evidence to support that any proposed device has the data to support the potential to achieve the intended benefit of improving mortality and morbidity in the extremely pre-term infant.
And that device related risks can be adequately mitigated to ensure that the benefit risk determination is at least as favorable as current standard of care in the NICU.
…
Alan Flake, Children’s Hospital of Philadelphia [10:34:10]
We set out to design the technology to maintain normal fetal physiology and to mimic as closely as possible the environment of the maternal womb.
By maintaining fetal physiology and extending gestation, this technology is expected to improve the survival and wellbeing of extreme premature neonates. An important safety feature of the technology is that it allows the neonates to be quickly transferred to the standard of care, if the technology fails for any reason.
The essential components of the artificial womb are first a sterile fluid environment maintained by continuous fluid exchange, that is fresh fluid in and waste fluid out. Second, a pump-less, low resistance, low surface area, arterial venous oxygenator circuit, powered by the fetal heart rather than a pump.
And third is the use of the umbilical vessels as a vascular conduit. Very simple in concept.
…
Alan Flake, Children’s Hospital of Philadelphia [10:37:21]
So why the lamb model? Most of what we know about fetal physiology has been defined in the lamb model and for the most part has been validated in our understanding of human fetal physiology and development.
The fetal lamb is the only model that I am aware of that is large enough at developmentally relevant time points to fulfill the surgical and mechanical requirements for development of the artificial womb.
The primary models are simply too small, 100 to 200 grams at developmentally relevant time points, with umbilical blood flow too limited to utilize current oxygenator technology.
…
George Mychaliska, University of Michigan Health [10:58:19]
We are currently in the midst of a prospective study, including other variables, including markers of morbidity. Clinical application would utilize existing NICU and ECMO platforms, with modifications such as perfluorocarbon filled lungs, which we have used in a previous clinical trial of congenital diaphragmic hernia patients on ECMO.
Early application of the artificial placenta on the first day of life, after risk startification, would be expected to reinitiate fetal circulation with minimal barotrauma.
For premature infants not captured on the first day of life and subsequently fail maximum medical therapy, the artificial placenta would be applied as a rescue therapy.
We recognize there are many ethical and regulatory considerations prior to clinical translation.
…
Mike Seed, The Hospital for Sick Children Toronto [11:07:04]
In conclusion, we have yet to achieve consistent physiologic, fetal circulatory parameters in our model.
We believe this is due to our circuit imposing abnormal cardiac loading conditions on the fetal heart, which is perhaps not surprising considering our use of devices that were not designed for this purpose.
However, we remain extremely enthusiastic about the potential of artificial womb technology and are about to embark on a new set of experiments using a third iteration of our circuit.
…
Alan Flake, Children’s Hospital of Philadelphia [11:18:32]
That’s one of the limitations of the animal model is that sheep are quite difficult to survive after any intervention in which they are not normally delivered and placed on ventilation, etcetera.
And that relates to their multiple stomachs, swallowing air when they’re on the ventilator, competing with their respirations, etcetera.
So we have survived four lambs after being in the system. One of them was followed up for over six months and we saw no obvious morbidity in the lab. Now that’s a limited assessment obviously.
We did do neurocognitive assessment in the lab and some other testing, but we could see no evidence of abnormality, but this isn’t, obviously, relevant to long term human morbidity after the use of the artificial womb.
And I think that’s going to rely on long term follow up of any subjects that are placed on the artificial womb for many years, actually to see what its long term effects may be.
…
Alan Flake, Children’s Hospital of Philadelphia [11:58:17]
I would respectably disagree with Mike. I don’t think that it’s size related, if you think about normal fetal physiology, the normal fetus at whatever size tolerates a pump less AV system. So it’s a matter of circuit specifications, circuit resistance, circuit volume, et cetera.
We’ve been able to maintain animals that are equivalent in size to the human infant, meaning in the 6 to 700 gram range, meaning lambs, for long durations on our system. And the Perth group was able to maintain them for approximately two weeks, although they did have some issues with maintaining physiologic flows for that period of time.
We’ve been able to maintain, as I said, a 700 gram animal for 29 days in fairly normal physiologic conditions.
So I don’t think it’s a matter of size. I think it’s a matter of the circuit specifications with respect to the pig model. I’ll have more to say about that tomorrow, but we’ve been able to rapidly convert pig fetuses that are human in size from placental support to circuit support with physiologic blood flows.
And, I’ll discuss more about that tomorrow, but it has not been a limitation in our system to run pigs for short duration physiologically.
…
George Mychaliska, University of Michigan Health [12:08:03]
It’s a great question. So I will say that we do need to– we don’t paralyze the animals, but we do give them benzos and some narcotics to keep them comfortable. And in those video clips, the animals don’t move very much.
And I didn’t capture in that video, we have early in our experience, we would cap the endotracheal tube. So it was more akin to sort of a tracheal occlusion model, but we’ve started leaving the perfluorocarbon to a meniscus, and we usually see that meniscus moving with simulated fetal breathing movements.
Now, obviously they have an endo tracheal tube in their trachea. So it’s not exactly the way it happens in nature, but they are moving that fluid. And, we’ve noted, and this is well known that lungs and a fetus need to be filled with fluid to stimulate normal growth and development.
…
George Mychaliska, University of Michigan Healt [12:12:07]
The way we’re envisioning clinical translation is twofold.
One way would be on the first day of life. And that would be with a clinical risk stratification system where we would preemptively put infants at a high predicted mortality on the device. In that application, based on our animal work, we believe that fetal circulation would be reinitiated and there would be minimal barotrauma from the initial resuscitation.
The rescue mode, I think we can all acknowledge, we may not capture all of the patients on the first day of life. And clearly extremely premature infants die at various time points.
On the first day, maybe the most premature from respiratory failure. But then later in their course, they may exceed maximal medical management. So those patients could be placed on the artificial placenta, their lungs filled with perfluorocarbon to protect their lungs, and continue the maturation process.
And I would acknowledge that fetal circulation likely would not be reinitiated, and there would be a greater degree of barotrauma. So this would be in my mind sort of extending what we think of conventional ECMO, to a more premature group of infants that definitely need it.
And so that’s why we also focused a lot of our work on developing non thrombogenic surfaces, because as we’re all aware here, we typically don’t provide ECMO for premature infants, even at 27, 28, 29 weeks.
…
Steven Krug, PAC [03:33:17]
I’m not an neonatologist, however, I care for a lot of a lot of children who’ve survived prematurity and I offer one observation.
First of all, the, the presentations today have been outstanding. But the scope of complications that we need to consider is actually, I think, broader than what was actually presented. And again, I think the presenters were focusing on the things that are the most common and or the most potentially severe.
It’s incredibly clear to me that survival is not the endpoint. And that survival isn’t necessarily what’s most important to families.
And one of the difficult issues we’re going to have here, which is certainly going to, I think, add a fair amount of time to trial, to then expansion to practice, is that there’s going to need to be some fairly extensive follow up on these infants for quite some time.
Certainly for me to be then able to say, you know what, this is the same, or maybe it’s better.
…
Robert Dracker, PAC [03:56:47]
So what I’ve heard from all the members is that number one, there is a concern with following the long term consequences of using this technology, and number two, from what I’ve heard, making sure that we are using the appropriate animal model, and assessing it fully before we undertake human studies.
…
Michael White, PAC [04:02:43]
We need to decide what is considered a reasonable expectation for improvement and where we want that outcome to be.
I don’t want to get into the information and the discussion that we’re gonna have tomorrow, but I think we need to have adequate data in an animal model that we can reliably get to whatever goal that’s going to be. I think four weeks is a reasonable expectation, but that’s me. No one has to agree with that.
So I think, I think I’m in agreement with what Dr. Nelson has to say.
I also wanted to make just one quick comment about the Berlin Heart and how that was approved. In the Berlin Heart, the choice was death versus ECMO or death versus the Berlin Heart, which is a very different circumstance than what we’re discussing here.
So it would be hard to use that same decision tree, uh, in what we’re discussing today.
…
Jeffrey Feinstein, Stanford University Medical Center [00:16:50]
I think we’ve talked about a number of different issues here in a number of different challenges, both for the families and for the providers and for their researchers. And we talked about the concept of effective informed consent.
One of the things that came up in one of the earlier presentations is we don’t actually even have a standardized nomenclature for what the babies are gonna be termed. So if you think about sort of all of the logistical pieces in this, and trying to make sure that all of the different families in all of the different centers get some version of similar information, similar approaches, similar promises, if you will, the concept of a centralized IRB, maybe quite effective here, the concept of potentially convening some version of an expert panel to determine what some of the nomenclature may be.
And for this particular space, which is brand new, the fact that somebody is gonna be first in with their clinical trial again, do we let them set the rules, set the nomenclature, set the endpoint, or should this be sort of a more global discussion?
So that first in and everyone subsequent is all using similar approaches such that people who are hearing about this, again, whether as a clinician or as a researcher, or as patient and least have some semblance of similar experiences.
…
Robert Dracker, PAC [00:23:14]
I think the important aspects of the informed consent process is that they be inclusive and have optimal clarity and explaining to the prospective parents what the risks and benefits are. And that the first in event occurs at a clinically competent center who is familiar with the technology.
…
Robert Nelson, Industry Representative [00:27:23]
Neonatology, I mean, we all know that if you really want to know the outcome, it’s going to take years, but that’s not possible here.
And so if you’re enrolling one at a time, you just need to identify some short term safety endpoints that need to be looked at, to then make a decision about continuing. And the difficulty is that this is a population who’s going to in fact suffer some of those same morbidities, independent of AWT technology.
So, if the first patient has, let’s say a grade two bleed, what do you do?
Now, you know, it’s going to be a very tough decision. And you’re not gonna know about chronic lung disease until you get out into the, a little bit further down the line, but I mean, this is maybe where some of the clinical data really needs to be developed what that baseline is, but, one case you wouldn’t want that to kill the technology. And so this is, this is going to be a very tough decision.
…
Sarah Hoehn, PAC [00:29:45]
Obviously the big things you wanna look at are mortality, bleeding, there are going to be risks of bleeding or risks of clots, infection, and growth.
You know, you saw a lot of the data in the animal data about how they continued to grow, but I think there would also be things looking at the side effects such as bleeding, but also looking at whether or not in real humans do the babies actually grow, because if they’re not growing, obviously then they’re not gonna continue to mature.
So that would be some of the more immediate safety endpoint you could look at.
And I think it’s really hard cuz it almost needs to be set up as a non-inferiority trial that it’s not worse than the standard of care, but the only way to approve it is under this prospect of direct benefit, which is really hard because we’re really trying to, what people are trying to do is prove that it’s not worse than the standard of care, but it’s hard to reconcile the noninferiority with this prospect of direct benefit in the absence of no human data.
And I do think it would have to be really important that there’s a very robust DSMB that’s looking at all the data in real time, probably on a weekly basis, just so everyone’s aware of any of the potential initial short term complications.
…
Andrew Farb, FDA [04:41:06]
I think the last three comment comments really get to the heart of this question and really address exactly what we’re looking for from the panel. And that is, early feasibility studies cast a wide net for information gathering, starting with proof of principle.
And then when getting to the adverse events, we’re looking for all of those, all the important ones that affect the outcome and get to the safety of an effectiveness of this device.
And then, but what we’ve heard in the last two comments in particular, is the interpretation of those events and attribution of those events to what might be directly related to the device functionality and what could go wrong and how they, the sponsors in developing the device, have been able to develop their device to address potential failure modes, and whether that’s successful in the actual first application of the device.
And then what may be events that may or may not be attributable to the treatment related to the device, but may reflect the natural history treating these very premature infants.
So, I wanted to thank the panel for those those comments.
…
Robert Dracker, PAC [04:50:28]
I wanted to mention that, uh, when a child is undergoing this therapy, the assessment of the child is probably going to be different than what the typical assessment would be of, of a child born at 22, 23 weeks gestation, as far as you know, on a ventilator, receiving hypera, watching the bowels, watching the lungs, things like that.
But under in this device, I think it it’s gonna have different safety issues and different points that we’ll have to be cognizant of to assess if the trial is experiencing an adverse event.
And then, I think as mentioned by Dr. Takima, is that the issue of a parent seeing their child within a bag for two to four weeks and hooked up in multiple ways could be emotionally very traumatic to the parents, obviously different than seeing a child in a sled being supported.
So I think these are all issues that first in human is going to be a very significant event, for everyone, both the physicians and providers involved and also for the parents obviously, and the child.
…
Robert Dracker, PAC [04:55:27]
Number one, the people developing these technologies are familiar with what adverse events might occur, not only based upon the animal model, but also with their experience in human beings and in neonates.
And then once we have that first in data, then we know what we can watch for, what safety endpoints have to be developed as we go forward and utilize other infants in these studies.
But the first thing is going to be critically assessed both short term and long term. And that the point that you are satisfied with the tolerance of the technology and the outcome of the technology will determine when you start enrolling additional subjects.
FDA commissioner at National Health Research Forum session
- Source: webcast by Research America
- Date: broadcasted Tuesday, September 19
Robert Califf, FDA [00:00:54]
We have Brian King now as a new leader and a much invigorated effort in the enforcement side and some major federal rules that should get finished this year, that are in the hopper, one prohibiting menthol in cigarettes and another prohibiting flavored cigars. And then a really big one that would be a draft, which is limiting the amount of nicotine in cigarettes, which could have a major impact on the almost 500,000 Americans that die every year from tobacco related illness.
I feel like always have to say that more than once. Because I think most people like me, when I first came to FDA in 2015, it just seemed like we had taken care of this problem. And, we all, I don’t think there’s anyone who believes that tobacco is not dangerous, or would argue about it causing illness. But, the fact is we still have millions of people using combustible tobacco, and now we have the threat of vaping affecting our teenagers in a major way. So a lot of work being done there in many ways.
…
Robert Califf, FDA [00:04:48]
We’ve taken a good, hard look at the clinical trials system. There’s a Reagan Udall Foundation report about to come out. And I can’t talk about exactly what’s in the report, but what I will say is at least from my perspective, if we look at, medical product development, phase one, phase two, phase three, the sort of development phase, I think that goes really well.
What, where we really have a gap, is after what happens at the end of phase three, these days, over half of our approvals are accelerated. And so we’re putting things on the market with a lot of uncertainty about exactly and whom is this product most effective and how does it compare to other products? And what’s the value in a health system spending $4.3 trillion a year, with the shortest life expectancy of any high income country now, and seeing a decline in life expectancy in this country.
And so we need participation that’s representative of the population at risk. And of course that means the traditional issues that we talk about with, race, ethnicity, sex, gender, but it also means age. And it means, where you live, one of the biggest factors evolving in the U.S.
…
Robert Califf, FDA [00:08:25]
We are the U.S. Food and Drug Administration. U.S. is 4% of the world’s population. It’s a global industry and we don’t control what happens in other countries.
And so when we look at our aggregate data, people have done a lot of talking about this, it doesn’t look very representative of the United States, but we’ve just done a pretty major effort to segregate U.S. enrollment from non U.S. enrollment.
And guess what? At least the initial look, even FDA regulated trials done by industry, U.S. enrollment looks pretty representative. It’s getting there like the NIH has already done. I think that’s a major achievement.
Now it raises another question. What do we expect for a diversity in a global population? There are eight billion people in the world, and we’re not the only country. So we’re going to need to have discussions about what our expectations are for clinical trials, but at least we’re straightening out, I think some misperceptions and always feel like we’re slow on giving credit when people have done hard work and made progress.
…
Robert Califf, FDA [00:14:33]
We are learning more and more about misinformation. I hope your panel came up with some great ideas. I mean, the things we know we all need to do is every individual needs to spend time every day being aware that many of our friends and neighbors are living in information ecosystem which is dominated by views of science and medicine that are incorrect. And we also need to have humility that it’s not like we have all the answers and that’s not what science is about.
So transmitting that we are dealing with uncertainty, we’re making our best judgements, but there are areas where we’ve done the right studies. And we know for example, that vaccination prevents death from and hospitalization from COVID, that’s just a fact. And, we need to be able to say that in a way that– and embrace it after we’ve spent the time to be professionally adept at it.
But what we also know is that individuals out there, the best way to correct misinformation is an interpersonal interaction. So it really will take a network of people.
At the government level, we are working hard to get better at saying things in plain language.
Back in the good old days, when I used to interact with the FDA as a clinician, FDA made a lot of decisions. It wasn’t necessarily a matter of public discussion. Now, every decision the FDA makes is a subject to 24 by 7 internet chatter from people who may have spent 10 seconds thinking about all the data and analysis that went into that decision.
So we got to explain what we do in plain language. And we have to be preemptive where possible, where we think something that’s important for public health is gonna be attacked.
I do want to emphasize, because it’s a matter of recent court proceedings, in no way are we suppressing the right of other people to speak. The First Amendment is the First Amendment for a reason in the United States. And, where the line is about the old adage of you can’t yell fire in the movie theater, where that line is related to public health has not been defined at this point. And so we have to be careful that we’re not suppressing people’s right to speak.
But I also think it’s incumbent upon experts and knowledgeable people to counter information that’s incorrect. That’s out there. With the other point of view.
But I would say, I’ve talked to all the experts I can find. I haven’t found one yet that believes that we have the formula for moving this in the right direction. So we really gotta keep working on it.
September 19, 2023
CDC webinar on “Preparing for the Upcoming Respiratory Virus Season”
- Source: Clinician Outreach and Communication Activity webcast by the Centers for Disease Control and Prevention
- Date: broadcasted on September 19, 2023
Question [00:53:58]
Is there any reason not to administer or coadminister vaccines together, such as decreased immune response or an increase in side effects?
Amadea Britton, CDC [00:54:23]
This is Dr. Britton. I can start to answer that question and happy to have Dr. Grohskopf or Dr. Wallace jump in as well.
So, coadministration is obviously incredibly important. As I mentioned in my presentation, there is good data that RSV vaccines and influenza of vaccines can be co-administered safely, and that they generate non-inferior immune responses when they’re given together.
Just as you know, with administration of any two vaccines that may have some reactogenicity, that there can be additional side effects, if you give two vaccines together. And so if you have a patient for whatever reason, you’re very concerned about having side effects, that could be something to discuss with them about whether they would want to space, but there’s no requirement to space and it is acceptable to administer both RSV and influenza and COVID vaccines at the same visit, especially in patients that you think might have a difficult time coming back for additional visits or at very high risk of vaccine preventable disease.
So I will let Dr. Grohskopf and Dr. Wallace add, if they have anything to add.
Lisa Grohskopf, CDC [00:55:40]
This is Lisa Grohskopf. I don’t have much to add to that.
There are also, for example, there’s guidance concerning if you’re giving, for example, two vaccines that might be more likely to cause a local reaction. Some vaccines, for example, the flu vaccines, the high dose and the adjuvanted, might be more likely to cause a local reaction at the site, to administer in general, give injectable vaccines at separate sites if they’re given at the same time, but sometimes people will choose to say, if they have two vaccines, they’re concerned about local reactions with giving them in two separate limbs.
Megan Wallace, CDC [00:56:16]
And this is Dr. Wallace. Nothing to add for me, as I said, in the presentation, you know, co-administration of vaccines sort of remains best practice. And so that’s what we’re recommending for COVID 19 vaccines.
But if you’re planning to administer with an orthopoxvirus vaccine, we have some additional considerations that are in our clinical considerations guide.
…
Question [00:56:43]
Can you please discuss recommendations about vaccination administration following an active case of influenza, COVID 19, or RSV, and specifically wait times between being diagnosed with one of those diseases and then receiving the vaccination?
Lisa Grohskopf, CDC [00:57:04]
This is Lisa Grohskopf, I can take that with regard to flu.
There isn’t a specific wait time that’s recommended. In general, for somebody who has a moderate to severe acute illness with or without fever, it’s generally recommended that they’ve recovered from that illness and that that’s something that’s common across most vaccines and is in the general best practices guidelines for recommendation.
There isn’t a specific wait period beyond that. But in general, you’d want to wait, particularly if it was a moderate to severe acute illness, until recovery.
Megan Wallace, CDC [00:57:39]
And this is Dr. Wallace. I will add to that.
So COVID is the same. We recommend that everyone wait until they’re feeling better and sort of they meet the criteria for discontinuing isolation.
But in addition, if they’ve recently had a SARS-CoV-2 infection, they can consider delaying their COVID vaccine by three months from its symptom onset. And that’s just, we think that there’s probably some protection still from the infection up to that point. So you can do that if you’d like.
CDC webinar with testing laboratories on respiratory viruses
- Source: Laboratory Outreach Communication System webcast by the Centers for Disease Control and Prevention
- Date: broadcasted September 18, 2023
Manisha Patel, CDC [00:05:45]
Our early indicators, which are ED visits, test positivity and wastewater for COVID 19 are actually declining. So this is sort of the first week or two that we’re seeing that, since this uptick that we were seeing before.
Our later indicators, hospital admissions, they do continue to increase, but at a lower rate than we were seeing in previous weeks. So that’s good news, but again, none of us know for sure if that’s going to be sustained. So we are continuing to closely monitor.
And then for RSV, we’re starting to see that increase in the Southeast. I’ll show you some data from Florida, but still it’s low nationally.
And then the third point is influenza activity still remains low.
…
Manisha Patel, CDC [00:11:13]
Here’s some RSV data, again, nationally, not too much activity, but, if you look at the Southeast, you squint, you can start to see a little bit of an uptick in our RSV activity. This is NREVSS data, and then Florida, really pulls it out into suggest that they are starting to see RSV activity.
And this is a normal geographic pattern, as many of you know, RSV starts in the Southeast and then spreads north and west.
…
Manisha Patel, CDC [00:12:47]
It’s an interesting question about skewing, because I do think that you’re right, that we don’t fully know the burden of COVID 19 in the U.S., because not everyone has access to tests. And there’s certainly a lot of changes that are happening behaviorally. People aren’t necessarily always testing when they have COVID like symptoms, like maybe they used to do in the beginning of the pandemic. So there’s a number of reasons that could be shifting.
But I do think for this year, in the past couple of months, it’s pretty consistent, because our data is coming for the lab testing data is coming from NREVSS, which are clinical laboratories that are submitting, so that data’s not picking up home point of care tests and never actually did.
So appreciate the question. It’s an important one, but I think we have enough information that the trends are interpretable and have been regular and interpretable in terms of the way the data is being submitted to CDC.
…
Lydia Atherton, CDC [00:19:40]
Most of these, EG.5, FL.1.5.1, and the XBB’s, those are all part of the F456L mutation grouping.
So predictions for the next two weeks would be that there are going to be very few changes numerically from the last report. XBB.1.5 is projected to decrease in proportion nationally, about by 2% of cases. Many viruses still contain the identical or closely related spike protein sequence for that variant.
And then for those lineages that encompass F456L, those are together, are comprising almost over 64% of viruses nationally. Within that group of variants, EG.5, which you can see here in yellow, that is the major component at around 25% and then HV.1, which you can see here in green, that’s the fastest growing variant nationally and is predicted to comprise about 8% of cases.
And then in terms of where we’re looking geographically in the Nowcast, XBB.1.5 has dropped below 3% of cases in all regions. And as I mentioned, HV.1 currently has the highest growth rate in each region, with doubling times from 18 to 22 days. Just to give you a range, proportions in each region are predicted between 3% in– and then up to 11% in the different regions.
…
David O’Connor, University of Wisconsin-Madison [00:23:11]
We’re going to talk today about indoor air sampling for respiratory viruses. And this has several advantages, some of which are obvious and others, a bit less. So, it’s very cost effective to sample an indoor space, such as a school cafeteria, an unhoused shelter, an emergency room, for respiratory viruses in the air. It’s also anonymous to the individuals who are contributing viruses that are detected in the air. And of course, as was alluded to earlier, it’s resilient to individual testing behavior.
The type of air sampling we’re talking about today uses a Thermo Fisher aerosol sense air detection instrument. This is a versatile and portable instrument that can be deployed immediately to new settings and has very simple ease of operations, such that in some of our schools, we have like fifth and sixth graders who are responsible for changing the air cartridges a couple of times a week.
So we have explored a variety of different types of use cases for indoor air sampling for viruses. Our– we got started using it as a way of monitoring virus transmission within and between communities. One example of this is doing K through 12 school monitoring for pathogens, including SARS-CoV-2, influenza and RSV as a way of understanding community risk.
We can also use the same technology as an early warning system for looking at settings that are at high risk for consequential outbreaks. So for example, we have a couple of air samplers running in a complex care long-term care facility.
And finally it could be used to identify novel virus threats. An example of this would be using this technology in international airports to look at the introduction of viruses of concern.
…
David O’Connor, University of Wisconsin-Madison [00:33:13]
We’re working with Gingko Concentric to incorporate air sampling into the CDCs traveler genomic surveillance program.
I’m sure some of you on the call are familiar with this and, might be aware of this as something that’s coming soon.
We’re working to increase the sensitivity, cost, and throughput of viral metogenomics so that we can make this a more reliable first readout of what’s present in an air sample.
We’re looking to make the detection itself faster by introducing point of source testing, as well as improving high throughput multiplex detection to be lower cost and faster.
We’re also working with a different type of air sampler to recover live virus so that we can also study infectivity as well as the presence of viral RNA.
…
David O’Connor, University of Wisconsin-Madison [00:36:18]
So going back a couple of years ago, my understanding is that the cue branch has worked with Ginkgo Concentric and what was formerly known as XpresSpa to do pooled PCR testing of arriving international travelers at a variety of international airports. So that’s been ongoing for a while. So when people arrive, they can opt into contributing a a nasal swab at a kiosk. They then get pooled and brought back into the lab for PCR testing and sequencing.
We’re looking to put the air samplers at those same kiosk locations, so that while people are registering for participation in pooled PCR testing, we will also be sampling the air at the same time, to see if we’re able to detect SARS-CoV-2 in the air and determine what genotypes of SARS-Cov-2 are in those samples.
September 18, 2023
NIAID officials on draft DURC and P3CO policy changes
- Source: webcasts of a National Advisory Allergy and Infectious Diseases Council meeting
- Date: broadcasted September 11, 2023
Hugh Auchincloss, NIAID [00:16:16]
There is also an RFI out to comment about some questions that are posed about the revision of our DURC and P3CO oversight policies.
The actual RFI put several questions out there to you. It does not include the draft of the proposed revisions, but I can tell you a summary of those, DURC, that’s Dual Use Research of Concern, used to up until now involve 15 pathogens and 7 deadly sins, as we called them. P3CO, that’s pathogens of pandemic potential, that’s the three P’s, care and oversight, C O, okay? That has been modified in the draft form where it used to be.
We would worry about enhanced pathogens of potential pandemic potential, if there was a high likelihood of increased transmissibility and high likelihood of increased virulence.
The new draft guidelines says moderate likelihood of enhanced transmissibility or moderate likelihood of enhanced virulence.
I think these are worth commenting on. They are going to have, I think, a very significant impact on how we oversight, how we do oversight for this kind of research.
…
Emily Erbelding, NIAID [00:13:05]
There’s a request for information published last week on changes to the policies for the oversight of Dual Use Research of Concern known as DURC, and also Potential Pandemic Pathogen Care and Oversight, the P3CO policy framework.
This is the effort to revise these these policies was primarily under the– it was the responsibility assigned to the Office of Science and Technology, the OSTP, in out of the White House and also the National Security Council.
The proposed policy will actually expand pretty significantly the amount of the number of pathogens that have to be on the DURC watch list. This is my read of the draft policy.
Now, the draft policy isn’t published in this federal guidance, or in the federal registry, but a lot of questions on areas of that might be unclear or might be difficult to implement, are targeted questions are asked. And so by October 16th, OSTP and the National Security Council would like to get input from the scientific community, people that are involved in biosafety, at the institutional level, and also investigators who work with some of these pathogens to get input on how this policy, the draft policy, maybe could be improved to make it workable in the future.
So that’s out there, it’s important. If you don’t think that you’re a stakeholder, your institutional biosafety committee might want to be, you might want to point them to this RFI. So that the policy that comes out on the other side to be implemented next year might is the best in terms of biosecurity, bio safety, and supports the best science.
September 15, 2023
CDC officials and NCHS BSC members at meeting
- Source: webcast of a Board of Scientific Counselors, National Center for Health Statistics meeting
- Date: broadcasted September 14, 2023
Brian Moyer, CDC [11:15:58]
Based on my personal conversations with Dr. Cohen, she is a big supporter of data and a big supporter of NCHS. And, while she’s bringing her own priorities to CDC, she’s also carefully building on the many efforts that are already underway across the across the agency. And she’s referring to this as no sharp turns.
Next slide, please.
As we discussed at our last meeting, there is a new initiative underway at CDC and it’s called the CDC Moving Forward initiative. And, as we discussed, the idea is to improve CDC by building on what’s working well and addressing opportunities for improvement, where they exist and, sort of in that spirit, in Mandy’s spirit of no sharp turns, we and all the other centers across CDC remain committed to this CDC Moving Forward initiative.
…
Jennifer Layden, CDC [11:33:22]
Around Dr. Cohen’s priorities, we’re very excited that data technology is of high priority to her. There are three kind of core focus areas that she’s identified. One of them is the readiness and execution for the fall and winter respiratory illnesses, the second around mental health and combating opioid crisis, and then the third supporting young families.
We are working really across all three of these. Just to speak to a couple of them.
One is in the space of the fall readiness. So ensuring we’re doing what we can, in the anticipation of COVID, flu, RSV, and other respiratory pathogens, our office is leading the effort to find and visualize and disseminate the data out to the public for the fall surge.
So really emphasizing importance of a coordinated, integrated approach, across the agency, to meet our mission.
…
Brian Moyer, CDC [11:38:39]
Looking forward just a bit, the 2023 America’s Children report will be available on September 27. And as you know, this report is coordinated by NCHS, but reflects collaboration across 23 federal agencies. So it’s quite the collaborative effort.
This slide highlights some of the key findings from this year’s report. So, please feel free to check that out when it becomes available on the 27th.
…
Amy Brown, CDC [02:48:16]
So we’re going to be able to collect two rounds of the survey for this year, from July to September, and then from October to December. It’s taking us a little bit of time to set up the approvals in the processes. But we expect we’re going to be in a full quarterly data collection schedule, next year in 2024. So each round is going to have at least 4,000 total respondents, which represent completed surveys, drawn from nationally representative samples.
A minimum of 2,000 is going to come from each of two commercial online panels that will collect data simultaneously, versus the KnowledgePanel, from Ipsos Public Affairs and AmeriSpeak from NORC at the University of Chicago. These are two of the largest panels in the industry.
Our goal is to achieve a faster turnaround time for the release of data compared to our NCHS core surveys. So once all the operational processes are in place, it should take about six months from the time we receive sponsored content to release data on national estimates.
…
Amy Brown, CDC [02:49:44]
Sponsored content must address at least three, these three priority areas, as shown here. The first being time sensitive data needs, areas where existing statistical resources are unavailable, not timely or of insufficient or unknown quality.
The second measuring public health attitudes and behaviors, cases where things are changing very quickly.
And the last being development work, which provides agencies an ability to do some developmental work, areas where their concepts are less clear or evolving, or they want to do some measurement that can inform future question design.
The guidance also describes the type of estimates that the rapid surveys are not well suited for. And these are things like estimates that are already produced by our cross sectional surveys, our core surveys, because this is not meant to be a replacement for those, low prevalence estimates, or estimates for hard to reach or low prevalence subpopulations. So we’re very clear, upfront, before we receive proposals from provider potential sponsors.
…
Amy Brown, CDC [02:50:53]
This slide shows a few examples of the wide range of sponsor topics and it really is a wide range that we’ve received, that we’ve included on our first round. They were submitted from a variety of different CDC centers, institutes and offices. These include chronic illness from long COVID, household use of two air quality products, HEPA filters in air purifiers, several different types of cancer risk topics, including genetic tests, sunscreen use and carcinogens and hair products, and exposure to intimate partner violence.
Next slide.
We’ve also partnered on this first round with OMB’s interagency technical working group on race and ethnicity standards. We’re helping them to test some alternative wording for proposed standard race and ethnicity questions. So in addition to our CDC partners, we also have one external partner, OMB as well.
…
Amy Brown, CDC [02:51:48]
And I’ll just conclude by saying that the initial data release from this first round is expected sometime this coming winter.
Data’s is going to be released on a variety of formats, including an online interactive dashboard set of web tables and restricted and public use data files.
…
Amy Brown, CDC [02:53:16]
I think that when– there has been a great of great level of interest. We put out a– we have a form to send an announcement out to all of the CDC centers and institutes. And we received very good attendance at a webinar to get some basic information. And then that was followed pretty quickly with a number of proposals.
And they really were a range of topics kind of all over the place. Because it’s a good a good opportunity to be able to– particularly if there’s some topics where they wanted do some development work, question design, this is a unique opportunity to be able to field that and get data back in a relatively for us timely manner.
…
Adena Galinsky, CDC [03:01:00]
This challenge has only gotten harder as you know, and has been particularly hard for NHIS FR’s as anti-government and anti CDC hostility has increased.
Second, they asked for more help overcoming overcoming access barriers to sampled addresses such as gated communities, locked buildings, video doorbells. In other words, a way to get a message over the castle wall, and convince the residents to lower the draw bridge down over the moat.
Third, there was a clear need for morale boosts, given the increased emotional labor demands of the FR job and the post COVID pandemic exhaustion and disconnection that so many of us have been facing, FR morale is pretty low. So this likely translates to higher FR attrition and training costs and lower response rates. So the FR’s asked for more encouragement, gratitude, and celebration of successes and more paid opportunities to connect with and get help from other FR’s and FS’s to power their work and lift their spirits.
…
Adena Galinsky, CDC [03:05:47]
The third initiative is a project to encourage and help more FR’s use the handwritten note technique that some FR’s developed and described to us. So when used correctly, the FR’s who pioneered it report, it can help FR’s contact respondents behind access barriers and convert reluctant respondents.
So we’ve created a new piece of stationary, the blank NHIS note card, whose front and back are shown here, that the FR’s can use for these notes and a motivational training module. And, we’re working on a printed job aid with sample note text adapted from real notes provided by the FR’s, to make the process of writing these notes easier.
…
Andy Peytchev, NCHS BSC [03:12:41]
On your more direct question about any negative sentiment against CDC, it can go both ways. It just depends on the person. And so varying, that seems like an intriguing idea. To what degree do you emphasize CDC versus Census Bureau and vice versa? I expect that all the FR’s are carrying census bureau badges, and that should be working to your advantage if that’s the concern.
Adena Galinsky, CDC [03:13:06]
Yes. And that is, that is something that certainly the more experienced FR’s did talk about that, about getting a sense for what to highlight, what to bring up, what to downplay, and it’s right. It’s something that right, you can’t know in advance. Exactly. But sometimes that it certainly is helpful to focus on the Census Bureau affiliation.
…
Alan Simon, CDC [03:17:30]
What’s going to be in the survey? It’s all the usual suspects, but some things, some new things and things were bringing back after some time.
So anthropometry or body measures, dental exams, labs, blood urine, we’re bringing genetics back for the first time in a long time, which is exciting.
Blood pressure, we’d hope to have three to seven year olds in there, which would be new and great work, but we found in our pilot testing that it didn’t go quite as smoothly as we’d hoped, so we really need some more pilot testing before we hit the field in a big way with blood pressure for that young age group.
Vision, hearing, DEX exams, spirometry is coming back after a while being out, nasal microbiome is new and exciting, dietary recall of course, one of the major reasons that we do NHANES, of course.
And I, I realized after I made the slides that, I forgot to add that medications are coming back too. Which is a sort of widely used part of NHANES.
…
Alan Simon, CDC [03:15:21]
It’s fundamentally the same in that it’s still a population based survey with in-home interviews and then bringing people out to mobile examination centers. That part isn’t gonna change. Next slide?
But of course we are updating some things and making, hopefully, making some improvements. Next slide?
So one of the major changes is that we’ll be sunsetting the trailers that you see on the right. Not only because they’re getting old and worn out, but also we’re moving to trucks. That’s not actually the truck on the left, but it’s a very old truck, so I thought it was kind of representative.
The idea is that a mobile examination center will now be a set of three trucks. And why are we doing this? The trucks are more nimble. They can set up and be torn down much quicker. That’s going to allow us to be in more than one location within a primary sampling unit. I think that’s going to allow us to move around a little bit and get closer to our respondents, hopefully increase our response rate. They also have a smaller footprint allowing us to maybe set up in places that we couldn’t previously.
Other improvements are we’re going to more primary sampling units in the U.S. each year. We’re increasing from 15 to 20. We had hoped it was gonna be 30, but it looks like that’s not going to be feasible. So we are increasing to 20 that still provides some improvement over where we were. It’s still 5,000 participants a year. We’re just spreading them out over more areas.
We’re changing from our primary sampling unit of counties to public use micro data areas or PUMAs that Census creates. These are more standard across geography, in terms of population size. And this actually provides more statistical power. We’re also going to decrease the number of participants in each household that we go to. Again, the idea is you spread out the sample more, and that provides you with better power than we than we have now, hopefully allowing us to create estimates for slightly smaller groups than before.
HHS officials and DGA members at third meeting
- Source: webcast hosted by the Department of Agriculture and Department of Health and Human Services
- Date: broadcasted on September 13, 2023
Janet de Jesus, HHS [09:02:44]
There has been recent interest in the status of the guidelines for alcohol. And we wanted to note that the development of recommendations for the next edition of the dietary guidelines has not yet begun including guidance on alcohol consumption.
The topic of alcohol is not being examined by this current committee. Evidence will be reviewed in separate processes and more information is available on our website on our related projects page.
…
Janet de Jesus, HHS [09:03:18]
The committee has six public meetings. The final meeting meeting six will include the committee’s presentation on their draft report. And we’ve asked that the committee submit the report by October 2024.
Following the release of their scientific report, HHS and USDA will begin the process to update the dietary guidelines to be published in 2025.
CDC officials and ACIP member at IDSA webinar
- Source: webinar hosted by the Infectious Diseases Society of America
- Date: broadcasted September 14, 2023
Hanna Kirking, CDC [00:13:51]
Right now, in the U.S., we started to see a rise in COVID 19 cases and then hospitalizations in late June and throughout mid-July, and where we’re at today in terms of the trends with where we’re going, is right now nationwide kind of test positivity seems like it maybe has now plateaued at kind of a potential early peak. ED visits are plateaued and hospital admissions are going up. And again, this pattern should be interpreted, realizing that we expect a slight time shift with these.
Here you can see there’s slight different patterns in different regions, but overall that’s the, the nationwide trend.
So next slide? This slide just shows the overall epi curve of hospitalizations throughout much of the pandemic. The hospitalization numbers are shown in the blue bars and these are weekly counts. The superimposed orange line is actually proportion test positive, and that one is using the Y axis on the right. And so you can kind of see the yellowish orange line relative to hospitalizations is back shifted a little bit to the left. And that reflects that difference that I was talking about.
Also in this slide, you can see kind of hospitalizations is still kind of on the upswing it seems like, realizing that there’s a reporting delay. But we’re starting to be hopeful that we may be peaking in terms of proportion positive. That’s a guarded hope, but it’s there nonetheless, just based on kind of curve and overall patterns.
Next slide, one more please?
All right. This curve shows percentage of emergency department visits where COVID 19 is diagnosed and it’s separated out by age. So the Y axis is the percent of the emergency department visits. The X axis is date or week. You can see here, I think the big takeaway here, also is that in a couple age groups, we’re starting to see the peak kind of leveling off.
And again, that’s kind of integrating various data with hopes that we might be reaching the peak of this increase we’ve seen the last couple months.
…
Keipp Talbot, ACIP [00:41:20]
Bye bye booster. We are no longer giving boosters and it’s going to be very difficult to stop using that word because that word has become pervasive.
We are currently giving the updated 2023-2024 vaccine.
We are beginning to think of COVID like influenza. Influenza changes each year, and we give a new vaccine for each year. We don’t boost each year. So it’s going to be difficult to start changing that terminology, but it is no longer a booster. It is now the current vaccine for the year.
…
Amadea Britton, CDC [01:26:35]
I can speak to the adults. And this is a critical concern. And I saw a lot of questions about it, where some of this is a little bit beyond the scope of CDC, unfortunately, a little bit hemmed in by what’s happening across the board.
But what I can say is that these vaccines are covered under Medicare Part D, which means they, because of the changes with the Inflation Reduction Act in January of 2023, they should have zero cost sharing under Medicare Part D.
That doesn’t address the issue of people that don’t have the Part D coverage. But, if you do have Part D they, regardless of the fact that they are prescribed under shared clinical decision making, they are covered with zero cost sharing.
In terms of private insurers under the ACA, they also are required to cover this, despite it being shared clinical decision making, because it will be on the adult immunization schedule. I know there have been some hiccups with that because that requires separate approval by ACIP. But we have tried to address that. And, we are definitely working with our other federal partners.
We have a banner up now on the website that basically says, this is part of the adult immunization schedule, even if it’s not on the actual chart yet.
But the one other thing there for providers to know is that even though it will be covered eventually without cost sharing by private insurers, they have up to a year from the recommendation to add it to their plan. So that’s part of what we’re seeing too.
So I think the good news is in the long term, we expect coverage for the adults to be very good. But, the– right now, as we’re kind of in this introductory period, it definitely is challenging. And we understand it’s a huge equity issue, and we’re definitely trying to work on it, and I will turn it over perhaps to Jefferson to talk about VFC.
Jefferson Jones, CDC [01:28:32]
So VFC, nirsevimab was voted to be included through resolution at ACIP in VFC. And we are expecting by the end or next month for those contract negotiations– I mean, it’s a goal, for those to be completed for VFC.
On the private insurance side, there is a lot more uncertainty we’ve heard about. Most inpatient hospitals are not VFC enrolled. And, we know tha bundled payments are an issue for nirsevimab. And then on the outpatient side, same as through ACA, it is required to be covered, but there is a potential lag for private insurance, as they have up to a year. And we have heard different timing based on different healthcare systems.
So unfortunately there’s not a easy answer to those questions, but we are working closely with AAP and with our liaisons from the insurance industry to ACIP to try and do, frankly, it’s just as, as best we can for a brand new product monoclonal antibody, this is a brand new class to be used this way, which is leading to a lot of implementation challenges, which are unfortunate, but at least we’re excited that we do have this product included in ACIP recommendations.
September 14, 2023
FDA spokesperson on whether new COVID shots are “boosters”
- Source: email from an FDA spokesperson
- Date: received September 14, 2023
On background: To clarify, these vaccines would not be considered “boosters” per se. These vaccines, as previously announced, would be updated with a new formulation for the 2023-2024 fall and winter seasons.
September 13, 2023
FDA spokesperson on status of oral phenylephrine after meeting
- Source: email from Cherie Duvall-Jones of the Food and Drug Administration
- Date: received September 13, 2023
If the FDA determines that oral phenylephrine is no longer considered generally recognized as safe and effective (GRASE) under the conditions of use in OTC Monograph M012: Cold, Cough, Allergy, Bronchodilator, and Antiasthmatic Drug Products for OTC Human Use (OTC Monograph M012), the FDA would issue a proposed order to amend OTC Monograph M012by removing oral phenylephrine as a GRASE active ingredient from that monograph. Stakeholders would have the opportunity to comment on the proposed order, including by providing additional data. During this time period, the marketing status of oral phenylephrine would not change. After considering all of the comments on the proposed order, the FDA would issue a final order on the GRASE status of oral phenylephrine for use as a nasal decongestant under the conditions of use in OTC Monograph M012.
The FDA has no further information to provide at this time regarding the timing of any decision the agency may make following the advisory committee meeting.
FDA officials and NDAC meeting participants on oral phenylephrine
- Source: webcast of Nonprescription Drugs Advisory Committee meeting
- Date: broadcasted September 11-12, 2023
Theresa Michele, FDA [00:46:19]
The main objective of today’s meeting is to discuss the efficacy of oral phenylephrine as a nasal decongestant. We will be including data that have become available since the committee last discussed this back in 2007. We’re also asking you to consider the potential safety and efficacy of higher than monograph doses of oral phenylephrine.
…
Theresa Michele, FDA [00:46:45]
Now, as you all know, phenylephrine is a very old drug. It’s been marketed for more than 75 years for a variety of uses and via a variety of different roots of administration. Anytime a product’s been on the market for that long it’s human nature to make assumptions about what we think we know about the product for the purposes of today’s meeting.
We’re asking you to put aside those assumptions and help us think critically about the data at hand, and in particular, what the data may or may not show.
…
Theresa Michele, FDA [00:50:44]
It’s not uncommon that we learn additional information about drugs that have been on the market for some time. And phenylephrine is no exception.
Some of the additional data was brought forward in two citizens petitions, one in 2007 and one in 2015. The 2007 citizens petition requested that the agency amend the dosages of both oral phenylephrine salts by increasing the maximum allowed dosage for patients 12 years of age and older. It also requested that FDA withdraw approval, or rather make it not GRASE, for use in children less than 12 years of age.
The 2015 citizens petition requested that FDA reclassify the oral phenylephrine salts as not GRASE due to lack of efficacy.
…
Theresa Michele, FDA [00:51:48]
Because of the additional data that had become available since FDA’s GRASE finding back in 1994, we convened an advisory committee in 2007 to discuss the safety and effectiveness of oral phenylephrine as a nasal decongestant.
At the meeting in 2007, the committee also considered the original studies supporting the effectiveness of oral phenylephrine. The committee noted that the results are not consistent across studies for nasal airway resistance and recommended that symptoms should be the essential primary endpoint. They also noted that evidence of efficacy consisted primarily of studies conducted 40 years ago, which is now 55 years ago. And it included fewer than 200 subjects who received oral phenylephrine 10 milligrams.
Due to the small size of the studies, they felt that near nasal airway resistance results may not be generalizable to a wider population. Based on this, the committee recommended that additional data be conducted, specifically, multicenter parallel, randomized, double blind placebo controlled trials, preferably with an active control, such as pseudoephedrine, to evaluate nasal congestion scores and symptom relief. They also recommended characterization of the phenylephrine dose response and dosing interval, comparison of the PK of single ingredient products versus multiple ingredient products, and a safety evaluation of the effects of phenylephrine on blood pressure.
I’m pleased to say that we now have much of the data that was requested by the 2007 advisory committee. And we are now bringing this back to this committee for consideration.
…
Theresa Michele, FDA [00:55:54]
An advisory committee is utilized to conduct public hearings on matters of importance that come before FDA to review the issues involved and to provide advice and recommendations to the commissioner. The commissioner has sole discretion concerning action to be taken and policy to be expressed on any matter considered by an advisory committee.
Now, as such, we are not asking you to make a GRASE determination today on phenylephrine as an oral decongestant. Rather, we are asking you to advise us on what you believe the data show in terms of effectiveness.
…
Ben Bishop, FDA [00:57:43]
Although the agency first took regulatory action in 1976, this action was based on the conclusions and recommendations of an advisory review panel, which was convened in November of 1972.
Not to be confused with other types of panels or advisory committees, that panel and others like it are known as DESI review panels. DESI stands for drug efficacy study implementation, and the DESI panels represented one of the agency’s pivotal first steps in a long process of rulemaking.
Almost 20 years later, the final monograph for nasal decongestants, part of the larger cold cough allergy bronchodilator and anti asthmatic monograph, was published in 1994.
…
Ben Bishop, FDA [00:59:00]
In 1962, a retrospective evaluation of drug efficacy was authorized by the Kefauver-Harris amendment. Notably, the law mandated that FDA evaluate effectiveness, whereas previous approvals had required only a determination of safety.
For non-prescription drugs, the drug efficacy study implementation or DESI review, began 10 years later when FDA assembled a list of over 400 active ingredients being marketed without a prescription and categorized them into 26 therapeutic categories. One of these became known as the cold cough allergy bronchodilator and anti asthma monograph, or CCABA monograph, and this included nasal decongestants.
…
Tracy Pham, FDA [02:46:38]
Phenylephrine had higher proportions of manufacturer and retail sales than pseudoephedrine. Since 2018, phenylephrine accounted for the majority of retail sales in both bottle and packages, and in sale dollars.
Retail sales of phenylephrine and pseudoephedrine decreased from 2018 to 2021, before increasing in 2022.
In 2022, phenylephrine retail sales represented 1.8 billion dollars, compared to half a billion dollars of pseudoephedrine retail sales.
…
Marcia Howard, CHPA [04:32:58]
Phenylephrine has played an important role in consumer’s temporary self-treatment of nasal congestion. It is the only available oral non-prescription medicine for nasal congestion that is sold without having to show an ID or to complete a log book.
Oral phenylephrine comes in both brand name and store brand versions. Nasal congestion is one of the most bothersome symptoms associated with colds and upper respiratory allergies and is linked to decreased work productivity and quality of life and to sleep disturbances.
Consumer satisfaction with oral phenylephrine is high. According to household panel data, half of American households rely on phenylephrine and over two thirds of these households chose to repurchase the medicines on average four times over the year, which is a strong indication of satisfaction.
…
Marcia Howard, CHPA [04:32:58]
Phenylephrine has played an important role in consumer’s temporary self-treatment of nasal congestion. It is the only available oral non-prescription medicine for nasal congestion that is sold without having to show an ID or to complete a log book.
Oral phenylephrine comes in both brand name and store brand versions. Nasal congestion is one of the most bothersome symptoms associated with colds and upper respiratory allergies and is linked to decreased work productivity and quality of life and to sleep disturbances.
Consumer satisfaction with oral phenylephrine is high. According to household panel data, half of American households rely on phenylephrine and over two thirds of these households chose to repurchase the medicines on average four times over the year, which is a strong indication of satisfaction.
…
Marcia Howard, CHPA [04:40:34]
Our position is that this is a safe and effective medicine and its removal will result in increased demand for pseudoephedrine and a shortage of FDA approved on shelf medications. It would have supply chain implications and would cause an increased burden on the consumers we serve and on the healthcare system.
…
David Spangler, CHPA [06:12:32]
If you do want to change to pseudoephedrine, one, you would need to be already licensed with DEA. If not, you’d have to be applying, have to institute certain security controls, compliance with state law requirements.
Then you would have to request your quota, request sgo in in the spring, manufacturing in May, procurement in April, you then get your quota, then some months later, and then as a practical matter of the retail level, typically they’re doing their planograms, what the store is going to look like, those get adjusted in the spring, and then implemented typically in the fall in most major retailers.
So you get a significant lag. Plus, as Dr. Howard mentioned, there’s a limit on the number of products that a retailer would be willing to carry behind the counter because of limited space.
…
Theresa Michele, FDA [07:44:34]
The thing that matters when you are dosing, a drug is how much of the drug gets to where it needs to be, and whether it is a high enough concentration to affect the receptor that it’s trying to affect to make the change.
So in this case, we need the drug to get to the alpha receptors in the nose so that they can constrict the blood vessels and reduce the amount of congestion. So the actual amount that’s absorbed is somewhat irrelevant. What we really care about is the fact that the concentration that affects the receptors is higher than the concentration that you can get into your body, because it’s extensively metabolized by the intestine.
…
Yunzhao Ren, FDA [07:45:48]
As a pharmacologist, we believe if a drug works, that means it should work at the site where it’s working for nasal congestion. You should, we believe that how the drug work at the nasal congestion is at the nasal mucosa, the amount or the concentration of the drug, let’s say following oral administration, should reach certain level to be efficacious or at least as potent as those animal studies, cellular studies, molecular studies indicating that concentration should work.
And the results show that, following the oral administration route, the amount of the phenylephrine, or the concentration of phenylephrine, failed to reach that threshold concentration, from the in vitro or cellular level.
There’s a concern raised in the morning by saying, ‘hey, phenylephrine has a very wide distribution, tissue distribution, which means when phenylephrine entered the human body, there could be some other organs which can absorb this phenylephrine, so that it can be enriched in certain organs— I shouldn’t use enrich, but distribute to those organs and bind to something.
But there’s no evidence to showing that the nasal mucosa, this tissue, can enrich, the phenylephrine amount of concentration at that local site.
And in addition as a pharmacologist, we believe that how this phenylephrine works is through adrenergic receptor, which is located in the blood vessels. And therefore in this scenario, the tissue distribution— I mean, let’s— the organ concentration, or irrelevant tissue distribution concentration, doesn’t matter here. What matters here is the blood concentration, the plasma concentration.
So we do measure, everyone here in this field measured plasma concentration, and it’s lower than EC 50 value.
So that’s why, from a pharmacology perspective, we can provide these evidence to support or explain the lack of efficacy from the clinical trials.
…
Martha Lenhart, FDA [00:44:23]
For clarification, three voting questions were posed at the 2007 NDAC.
For the first voting question, the advisory committee disagreed with the statement that phenylephrine in a 10 milligram immediate release formulation has been shown to be effective when dosed every four hours for the symptomatic treatment of nasal congestion and that no additional studies are needed to support its effectiveness. In other words, did it meet GRASE standards? Two voted yes. 10 voted no.
The second question was worded. Given the available data that exists, the evidence is supportive that the 10 milligram immediate release formulation may be effective. 11 voted yes, one voted no.
And the third question asked, whether additional studies are needed to assess the efficacy and safety of higher doses. Nine voted yes, three voted no.
In conclusion, the committee recommended that additional trials be conducted, specifically multi-center parallel randomized blinded placebo controlled trials, preferably with an active control to evaluate nasal congestion scores and symptom relief.
…
Martha Lenhart, FDA [00:45:49]
Since the 2007 NDAC, more data had become available. Next slide, please.
Certain clinical pharmacology information presented yesterday by Dr. Ren was not available to the 1970s DESI panel. This includes that only parent phenylephrine, not its metabolites, is active.
We note discussion yesterday about the bioavailability of phenylephrine.
Due to the extensive first pass mechanism, only a fraction of the orally administered dose is present as parent phenylephrine in the systemic circulation, the Cmax value of parent phenylephrine following an oral dose of 10 milligrams is low. About one nanogram per mL.
One nanogram per mL is approximately one third of the in vitro alpha one adrenergic EC 50 value because the blood vessel is the target organ and the site of action for parent phenylephrine. The plasma concentration of parent phenylephrine is clinically relevant.
This peak plasma concentration is unlikely to achieve a pharmacologic effect in the nasal mucosa needed for nasal decongestant. Both the PK and PD data suggests that a much higher dose of oral phenylephrine may be needed to achieve a nasal decongestant effect.
…
Martha Lenhart, FDA [00:47:51]
The original efficacy studies conducted prior to the 2007 NDAC do not meet today’s trial design standards. For example, clinical and statistical methodology issues of these studies included small study sizes that limit generalizability and inconsistent results across early studies suggesting possible data integrity issues, and of primary importance, the use of unvalidated nasal airway resistance or NAR for efficacy assessments.
In contrast to NAR, nasal symptom scores are the gold standard as an endpoint because they directly measure the symptom of interest. Every drug approved over the past 30 years in the cough cold allergy space have demonstrated to be effective based on nasal symptom scores.
…
Martha Lenhart, FDA [00:49:22]
More recent studies consisting of multicenter parallel, randomized blinded placebo controlled trials also showed that a 10 milligram dose of phenylephrine was not significantly different from placebo.
In summary, the new data appear compelling that the monograph dose of oral phenylephrine results in no meaningful systemic exposure and no evidence of efficacy.
…
William Figg, NIH [00:55:52]
Second, there was a lot of trying to confuse things yesterday, in my opinion, for CHPA’s discussion about metabolites.
First pass metabolism does not result in the parent drug being in the systemic circulation and bioavailability is really only the parent drug in the circulation, so that 1% is accurate or close to it.
So, both of those points suggest the concentration of phenylephrine being achieved in the circulation is substantially low.
…
Maria Coyle, NDAC [01:28:12]
If I were to do a short summary of what we have discussed to this point, I think several panel members have mentioned that they do believe that the concentration of drug, of parent drug, that is actually reaching the tissue in the nasal passages is low.
That overall the later studies do seem to provide some strong evidence that the phenylephrine at 10 milligrams may not be effective, is likely not to effective in relieving nasal congestion, at least in the population studied.
That there seems to be some agreement that the populations of patients with seasonal allergic rhinitis and those patients with cold symptoms may may overlap. And so not an unreasonable study population for those later trials, as well as some clinical context around what might be, most of what might be considered an effective treatment and how that effectiveness might be assessed.
…
Mark Dykewicz, NDAC [01:32:55]
In practice, the major potential complication of uncontrolled nasal obstruction might be the development of bacterial sinus infections. That doesn’t happen very often, but if you are looking at trying to maintain the patency or the openness between the inside of the nose and the sinus cavities to avoid mucus accumulation and possible development of a bacterial sinus infection, you certainly would want to achieve that or try to achieve that with an effective treatment. And oral phenylephrine is not going to do it.
So, there would be alternatives, such as intranasal decongestant sprays that for short term might work better. It would be off label. One might consider a nasal corticosteroid to help reduce congestion swelling within the nose.
But I think, um, are there clear cut studies that would prove that some of these alternative treatments are reducing the risk of developing bacterial sinusitis with the need for antibiotics and potential other complications? We don’t have studies that clearly demonstrate that.
…
Maria Coyle, NDAC [02:16:26]
So question two for our vote, do the current scientific data that were presented support that the monograph dosage of orally administered phenylephrine is effective as a nasal decongestant?
If yes, discuss what data you consider supportive, if no discuss what additional data, if any, are needed to assess phenylephrine pharmacokinetics or efficacy.
…
Jessica Seo, FDA
[02:24:28]
There were 0 yes’s, 16 no’s, and 0 abstentions.
…
Maria Coyle, NDAC [02:36:48]
I also voted no, for all the reasons stated.
I think we, we clearly have better options in the over the counter space to help our patients. And the studies do not support that this is an effective drug and delaying care or other negatives associated with care far outweigh you know, any potential, even in the future, if this drug were at different doses.
So I would not be in favor of additional studies at this time, along with my fellow panel panelists, who stated the same.
…
Karim Calis, NDAC [02:40:26]
We already know how this drug works. We already know its mechanism action. We already know what this class of drugs does. We just know that in its current form, in the dosage form that is currently provided at the current dosage, that you don’t. You have very low systemic exposure.
So, if we push the dose, it’s possible that you might get additional systemic exposure. But with that, we already know that we will probably very likely encounter additional cardiovascular effects, just as we would do from the entire class of those drugs.
So I think that would be the, the wrong thing. And I don’t think that the data would support that.
Could there be some efficacy at much higher dosage, possibly? But with the corresponding increase in potential cardiovascular effects and safety issues.
…
Maria Coyle, NDAC [02:48:36]
I’m hearing a broad consensus that the advisory committee members do not necessarily support a higher dosage be explored for OTC use.
…
Maria Coyle, NDAC [03:04:27]
I just want to summarize what we’ve heard thus far.
I think concern that any change in status for OTC phenylephrine be communicated clearly that, the public be reassured as to a lack of effectiveness or a lack of efficacy as the driver for this change, rather than safety concerns.
I think recognizing that some patients may be very in tune to the ingredients of their OTC products and may be very concerned that this product is not going to potentially be available. And maybe on the flip side, patients who are less in tune with the individual ingredients and may in fact not even be able to discern a difference.
I think also recognizing that we’ve been discussing sort of maybe an assumption that phenylephrine would be withdrawn from the monograph, while I want to acknowledge that that’s not really what we have voted on, per se. And so the FDA will have to make that determination.
But regardless, I do think information about this meeting and this deliberation of the advisory committee is out in the media, and maybe, uh, reaching the level of awareness of many of our patients. And so regardless of the outcome of these deliberations, perhaps some careful communication needs to happen, and that should probably happen at multiple levels, reaching providers, patients, consumer groups, and maybe in a variety of formats.
September 12, 2023
CDC, ACIP members, and companies on updated COVID vaccines
- Source: webcast of Advisory Committee on Immunization Practices meeting
- Date: broadcasted September 12, 2023
Demetre Daskalakis, CDC [10:26:24]
I’ll echo that we’re also aware that there’s a lot of interest in having non mRNA vaccine options available. And we also look forward to the potential authorization of the updated vaccine.
It’s important to note that the voting language that is going to be presented later today is inclusive of FDA licensed or authorized updated monovalent XBB containing COVID 19 vaccines, including those that may be licensed or authorized in coming months.
So this would allow such vaccines to be incorporated into programs immediately following FDA regulatory action. And that won’t require that ACIP be reconvened. So I hope that this will facilitate the availability of the Novavax vaccine once FDA has reviewed and potentially authorized.
…
Natalie Thornburg, CDC [10:44:20]
It’s kind of evolving in two different, I don’t want to say clades, but two different versions of BA.2.86 right now.
There are two U.S. sequences that are highlighted with yellow arrows. So one that was detected in Michigan and another sequence that was detected in Ohio.
Next slide please.
So BA.2.86 has more than 30 amino acid substitutions in spike in comparison to XBB.1.5. And as far as the sequencing goes, that’s a similar change in amino acid of spike during that Delta to Omicron shift.
There’s variations between sequences due to missing data and sequencing artifacts, but then there also may be some variations in it, in some of the viruses themselves.
…
Natalie Thornburg, CDC [10:45:21]
Again, it was first detected in specimens collected in late July 2023. And as of last week, there were seven clinical specimens, seven sequences, in seven U.S. states, and then there was one additional state detection in wastewater.
We may have a couple more this week and in coming weeks, but the take home message is we have a very small number of viruses detected in the United States thus far. And as of last week, it had been detected in 10 different countries.
We’re still dealing with a fairly small number of sequences.
…
Natalie Thornburg, CDC [10:51:03]
So as a reminder, um, more than 90% of circulating viruses are XBB lineage viruses with an additional, one to two substitutions in RBD, I’m sorry, this slide is not correct, but okay.
More than 90% of circulating viruses are XBB lineage viruses with one to two additional substitutions. BA.2.86 is a newly detected lineage with 30 amino acid substitutions in spike.
Thus far the number of viruses detected is still low. Sequence numbers are too low to calculate proportion though, so we don’t know if BA.2.86 will be of any significant circulation.
Preliminary pseudovirus neutralization data generated by multiple labs do not indicate a large reduction in neutralization activity.
…
Natalie Thornburg, CDC [10:52:11]
CDC has generated two authentic isolates of BA.2.86. One confirmed and one putative.
We are in the process of distributing BA.2.86 viruses to multiple labs to do transmission studies, more neutralization studies, against lots of different kinds sera.
And then we have another putative isolate, which is from a slightly different version of BA.2.86. We’re also locally working on titrations before neutralization studies.
…
Fiona Havers, CDC [11:05:46]
In summary, next slide, hospitalization rates have increased in all age groups since mid July. Hospitalization rates remain highest in older adults and in young infants, less than six months of age.
Most children under five hospitalized COVID 19 illness have no underlying medical conditions. A higher proportion of hospitalized children in adolescents in older age groups for those 5 to 17 years have underlying medical conditions.
And not surprisingly, most hospitalized adults have multiple underlying medical conditions.
COVID 19 continues to cause severe illness, with a substantial proportion of patients being admitted to the ICU in all age groups and clinical outcomes. While it varies a little bit by age group, are generally comparable to influenza associated hospitalizations, and most children and adults hospitalized for COVID 19, since January 2023 had not received a bivalent booster prior to hospitalization.
…
Fiona Havers, CDC [11:37:20]
We are collecting data at the time. Right now, we don’t have any data specifically on those infants who are hospitalized, but that is something that we’re looking into in, in data collection, on maternal vaccination of hospitalized infants is ongoing at the moment, but I apologize, I don’t have that available today.
…
Fiona Havers, CDC [11:45:37]
We do have data on that. We collect symptoms on all of our— when we do the medical chart review, I would say that the vast majority of children under five presented with respiratory symptoms who are admitted with a positive SARS-CoV-2 test.
And I will say that the data that— I think that most children are having respiratory symptoms, they are, some of them are being admitted with fever and other things. I don’t have a breakdown of symptoms on the slides here, but I’m happy to provide that after we do collect those data.
I would say, generally speaking, respiratory symptoms, such as cough, fever, shortness of breath, and then also symptoms like bronchiolitis in younger children are fairly common, but I don’t have a breakdown on these slides here, but I think that most of the children that we’re talking about here today, including among young infants, do have respiratory symptoms.
…
Filip Dubovsky, Novavax [01:14:31]
So the Novavax vaccine filing is under active review by the FDA. So this slide includes some forward looking statements, pending final authorization.
We understand our vaccine will be indicated for individuals 12 years of age and older, consistent with the age indication of last year’s vaccine. The vaccine will be distributed in two vials per carton, with five doses per vial, so each carton contains 10 doses, and the dose volume is 0.5 mls per dose. The same dose is used in all authorized age groups.
Our product is ready to use requiring no reconstitution and can be administered with standard needles and syringes routinely stocked in vaccine clinics. And the vaccine is shipped and stored as standard refrigerator temperature, and currently has a nine month shelf life, and is to be used within 12 hours of initial puncture of the vial.
In discussion with the FDA, we understand the single dose will be indicated for people who have been previously vaccinated, irrespective of which vaccine they received, and a two dose series 21 days apart, is to be used for those who have not been previously vaccinated.
…
Kayvon Modjarrad, Pfizer [01:34:18]
We have not had any use as of yet, but we will have a vaccine available as early as tomorrow in the U.S. in some locations.
…
Frances Priddy, Moderna [01:40:22]
So the list price for our vaccine is 129 per dose. Thank you.
…
(unclear), Pfizer [01:40:39]
The list price for Pfizer vaccine is 120 dollars per dose.
…
John Trizzino, Novavax [01:41:03]
The list and/or WAC price that we refer to, ours is 130 dollars per dose, which in industry conditions is subject to contract pricing and discounts. Also of note is that our contracted price with CDC is 72.50 per dose.
…
Matthew Daley, ACIP [01:43:49]
I have heard from small private practices about a minimum order amount, something like 200 doses. And I just think that creates barriers.
So I would ask all the manufacturers to consider reducing what the minimum amount that practices need to order, just because that’s a significant financial outlay, maybe 20,000 dollars, and it’s for a practice who might need to buy multiple doses for multiple different age ranges, for example, a small family medicine practice. And so then that just presents a barrier.
…
Megan Wallace, CDC [01:56:31]
During our discussions, the work group asked to investigate if young people with no underlying conditions, were still having severe illness from COVID 19. We know that that underlying conditions put you at risk, for higher risk, sorry— put you at higher risk for severe COVID 19 outcomes. And that the percent of the population that has underlying conditions differs dramatically by age.
To evaluate the burden among those without underlying conditions, we looked at the percent hospitalized for COVID 19 that have no underlying conditions by age group, which is the first column, and of those hospitalized with no underlying conditions, what percent were admitted to the ICU, which is the middle column, the final percent of those admitted to the ICU— and finally, what percent of those admitted to the ICU had no underlying conditions, which is the far right column in each of these categories.
We see that those without underlying conditions are progressing to severe illness, though we should note that these percentages should be interpreted with the understanding that children have a lower probability of having underlying conditions overall.
I also want to mention that these findings of people ages six months to 49 years with no underlying conditions progressing to severe outcomes due to COVID 19 was confirmed in other CDC platforms.
…
Megan Wallace, CDC [02:01:13]
In summary, COVID 19 burden is currently lower than a previous points in the pandemic. However, the absolute number of hospitalizations and deaths is still high.
Although hospitalization rates are currently low, we have seen rates increase in recent weeks and anticipate further increases as we enter respiratory virus season.
Infants and older adults have the highest COVID 19 associated hospitalization rates, children and adults with no underlying medical conditions still experience severe illness due to COVID 19.
We saw in Dr. Saydah’s presentation earlier that post COVID conditions are common following SARS-CoV-2 infection, decrease with time since infection, and have decreased since the start of the pandemic. People of racial and ethnic minority groups continue to be disproportionately impacted by COVID 19. High proportions of underlying conditions may put certain groups at increased risk for severe outcomes due to COVID 19. Next.
When asked is COVID 19 disease among persons six months and older of public health importance, the majority workgroup opinion was yes, next.
…
Megan Wallace, CDC [02:20:30]
COVID 19 vaccine benefits are anticipated in all age groups, but the benefits of COVID 19 vaccines vary by age and incidence of COVID 19 hospitalizations.
The benefits outweigh the risks in groups for which which risk of myocarditis is highest.
Modeling projects more hospitalizations and deaths are averted when updated doses are universally recommended compared to no recommendation or recommendation only for person 65 years and older.
…
Megan Wallace, CDC [02:24:12]
This slide shows intent to get a new updated COVID 19 vaccine as of August. 42% of respondents reported that they definitely will or probably will get the COVID 19 vaccine this fall. Next.
Based on data from the bivalent vaccine uptake and intent, we see that intent is highly related to receipt of previous COVID 19 vaccine doses. Those that had a past COVID 19 vaccination were more likely to have received a bivalent vaccine dose while the majority of the unvaccinated reported that they probably or definitely will not get a bivalent vaccine dose. Next.
And when we look at the top concerns or issues regarding the bivalent vaccine, among those that reported that they probably or definitely will not get the vaccine regardless of past vaccination status, the most commonly reported concern was unknown serious side effects.
Next, this slide shows reported confidence in vaccine safety for COVID 19 vaccine, influenza vaccine, and other routine vaccines. Confidence in vaccine safety is higher for influenza and other routine adult vaccines than for the COVID 19 vaccine, with only about half of respondents reporting that the COVID 19 vaccine is completely or very safe. Next.
…
Megan Wallace, CDC [02:27:36]
This slide shows fall vaccination intent by age group.
We can see that the vaccine intent increases by age, with those ages 65 years and older being the most likely to report intent to vaccinate. This trend is also seen with other vaccines, such as flu.
Next.
And this intent to get a fall COVID 19 vaccine mirrors the uptake we saw with the bivalent doses, with older adults, having a much higher coverage than younger adults and children.
Next.
Intent to get a new updated COVID 19 vaccine varies some, but not substantially, by race and ethnicity.
…
Megan Wallace, CDC [02:32:17]
There are still barriers to implementation. There are now three seasonal vaccines and preventative products, including COVID 19 vaccine, influenza vaccine, and RSV vaccine and preventative products, which means there are more vaccines to manage, limited storage space for more vaccines, and more opportunity for vaccine administration errors.
Providers will need to adapt to new cap and label colors, and all three manufacturers now have products with blue caps, introducing opportunity for error. Next.
…
Megan Wallace, CDC [02:35:30]
In summary, COVID 19 vaccination is a cost effective intervention, particularly in persons ages 65 years and older in which the vaccine is cost saving.
Cost effectiveness estimates in those ages 50 years and older were robust to input changes across plausible ranges.
Cost effectiveness estimates in those 18 to 49 years were sensitive to changes in inputs.
If vaccine effectiveness or hospitalization rates are higher than anticipated, the cost effectiveness estimates would be more favorable.
Cost effectiveness estimates are not yet available for the pediatric population.
Next, for equity we considered, if the intervention is a reasonable and efficient allocation of resources across all populations. Next.
COVID 19 vaccination is most cost effective in older adults in which disease burden is highest compared to younger adults. COVID 19 vaccination is likely more cost effective in populations with risk factors, such as underlying conditions, which increase their probability of hospitalization due to COVID 19.
Additional work is ongoing to evaluate cost effectiveness in the pediatric populations. Next.
When asked if the 2023-2024 COVID 19 vaccine is a reasonable and efficient allocation of resources, the majority opinion was yes, with a minority opinion of probably yes. Next.
…
Megan Wallace, CDC [02:43:43]
Finally, we have an optional— we had an optional second bivalent dose for those ages 65 years and older. We do not have an additional dose recommendation for the 2023-2024 vaccine at this time. We will monitor the epidemiology and vaccine effectiveness to determine if additional doses are needed.
…
Megan Wallace, CDC [02:38:47]
The work group considered non universal policy options with considerable discussion around the magnitude of benefits in the young, healthy population. As part of these deliberations, the work group requested additional data on severe illness due to COVID 19 in those with, and without underlying conditions, there was no group that clearly had no risk of severe illness.
Additionally, the vast majority of the U.S. population had an underlying condition that would qualify under a risk based recommendation, prevalence of overweight and obesity alone account, or is over 70% in adults.
A risk based recommendation would not allow access to COVID 19 vaccines for all that wanted them. Shared clinical decision making could create barriers to vaccination and may not effectively target those at highest risk.
COVID 19 epidemiology remains uncertain and non universal recommendations would need to be quickly revisited if there was an increase in burden. There is currently still substantial COVID 19 disease burden and simple stable recommendations may increase vaccine coverage over time.
The work group emphasized that COVID 19 recommendations should be reviewed on an ongoing basis as more is learned about COVID 19 seasonality and disease burden in the future.
…
Megan Wallace, CDC [02:40:08]
Burden of severe illness due to COVID 19 is lowest among children ages five to 17 years, despite lower burden relative to other age groups, hundreds of deaths due to COVID 19 occurred in this age group in 2021 and 2022.
Half of pediatric COVID 19 deaths were in individuals with no underlying conditions. The number of COVID 19 associated hospitalizations and deaths in this age group are comparable to the burden seen in other vaccine preventable diseases for which there are universal recommendations. There are potential additional benefits of vaccination, such as prevention of post COVID conditions. And the potential for reduced school. absenteeism.
Risk of myocarditis appears lower than the risk observed following the primary series doses, which may be due to the increased interval between doses. However, certainty is limited by relatively lower sample size of booster recipients in VSD.
The future COVID 19 epidemiology remains uncertain and the low disease burden we are currently seeing may not last.
After a robust discussion, the work group was supported of a universal recommendation at this time.
…
Melinda Wharton, CDC [03:15:46]
So the vote language as proposed, the intent of it is to cover for the upcoming season, the XBB containing monovalent vaccines as they are authorized, either under emergency use authorization or approved by BLA.
There is, as has been discussed today, one product, which according to the manufacturer remains under review, and we anticipate will likely be authorized soon.
The available information has been presented today. As far as I know, no additional information will be available, that would be able to be presented at an upcoming meeting, following regulatory action.
So, we certainly could reconvene the meeting, we always can reconvene ACIP if it feels necessary, but given the fact that no additional information is expected to be available, it feels like this is the kind of vote that we can move to a more normal cadence of things such as we do for recommendations like for influenza vaccine, where we don’t necessarily need to reconvene the committee when additional products are licensed under existing recommendations.
…
Georgina Peacock, CDC [02:50:25]
The federal contracts that have been modified in order to hasten delivery of the 2023-24 COVID 19 vaccines within our public health infrastructure for both children and adults will allow us to have the first doses available within 48 hours of the expected recommendation.
There will also be the retail pharmacies that have been contracted to provide doses for uninsured Americans through the Bridge Access Program, will also have availability within about that same time period, and we are expecting the commercial insurance will—commercial product will be expected around that same timeframe as well.
…
Georgina Peacock, CDC [02:51:35]
So typically the Affordable Care Act requires that insurers cover most ACIP recommended vaccines without cost sharing, by the next coverage year. COVID 19 vaccines are recommend— have been recommended on schedule since February 2023.
However, in addition to this, for COVID 19 vaccines, specifically in the CARES Act, there was statement that expedites coverage of COVID 19 vaccines, so that they are available immediately upon authorization under EUA or approved under a BLA. And you can see the more detailed information right here.
…
Georgina Peacock, CDC [02:52:19]
So people with Medicare and Medicaid will also have access to COVID 19 vaccines at no cost.
COVID 19 vaccines are covered under Medicare Part B without cost sharing, and the Inflation Reduction Act that was passed in August of 2022 eliminates cost sharing for all ACIP recommended vaccines under Medicaid and Medicare Part D equivalent plans and guarantees that nearly 50 million Medicare beneficiaries and more than 80 million Medicaid beneficiaries will have access to all vaccines recommended by ACIP without cost sharing.
…
Evelyn Twentyman, CDC [02:57:10]
The retail pharmacies in the Bridge Access Program are using three different approaches to maximize access to COVID 19 vaccines.
CVS plans to administer doses within both their storefronts and minute clinics. Walgreen’s plans to administer doses in both their storefronts and at offsite events, targeting areas of low access and low uptake.
eTrueNorth is a pharmacy aggregator that subcontracts with smaller pharmacies intended to reach lower access areas without other coverage within the Bridge Access Program, their discussions with additional potentially participating pharmacies are ongoing.
…
Megan Wallace, CDC [03:04:23]
So that you have the option to wait for three months, but it is not a requirement. So I think, as soon as they’re feeling better, they can get the vaccine if they want it, but they can also choose to wait.
…
Megan Wallace, CDC [03:21:25]
We’re recommending a two month interval, so two months from your past dose, you can get this vaccine.
…
Evelyn Twentyman, CDC [03:19:17]
There is indeed, uh, later this week, vaccines.gov will be updated to include a filter for Bridge Access Program site. In other words, all sites participating in the Bridge Access Program through which no cost COVID 19 vaccines can be found.
…
Pablo Sanchez, ACIP [03:26:54]
I’m not for a universal recommendation at this time.
I certainly think that those aged, the elderly, adults whether they’re 65 or greater than 55, should, I would recommend that, as well as certain risk groups, certainly the immunocompromised, in pregnancy, but I think that we need to be— we need to be aware and let the public know that the data on children is not there. And for that, I think that discussion needs to be had. So I think in non-high risk groups, I would favor a shared decision making. And, and again, in even the concern for the— for the 12 or 15 to 39 year old, the myocarditis risk, I recognize that— that it hasn’t been seen with the bivalent dosing, but the uptake has been low for that.
Well, so I think we need to be— we really need to level with our patients and say, what is known and unknown, rather than make a complete recommendation, especially for some groups that there are limited data.
…
Matthew Daley, ACIP [03:29:15]
There was some concern that the work group entered its to deliberations this summer assuming that a universal vaccination strategy was the obvious policy choice, but I just want to reiterate that that was very much not the case. The work group reviewed this as an opportunity to reevaluate the vaccination program. And we essentially started with a blank slate.
And so related, we, the work group, asked our CDC colleagues to update and present data on disease burden by age group for those with and without chronic medical conditions. And that was the most persuasive line of argument for me, knowing that there were deaths, including in children, including in those without chronic conditions, and my perception is that that those deaths are vaccine preventable.
And when we asked for this burden data, the focus was on serious disease, including hospitalization, ICU, admission, and death, and Dr. Wallace summarized all this for us and, and suffice it to say that the disease burden does very greatly by age, but there is serious illness, death across all age groups, including among those without underlying medical conditions.
So there may be a day where we revisit a risk based strategy. We always should consider this, but in order for that to be a desirable approach, I think we need to feel confident that disease burden in those not at risk, we need to be quite low and that’s low in absolute terms of cases of serious illness and death, but also low in relative terms relative to the burden of disease, for other diseases against which we have a universal vaccine recommendation.
…
Beth Bell, ACIP [03:31:49]
I think today we’ve heard a wealth of evidence about the risks, the benefits, extremely comprehensive dealing with the issue, and I, to Dr. Daley’s point, I think that it indicates there’s all kinds of robust information that show robust benefits of vaccination on severe illness on death, probably on long COVID.
And, so with a reasonable safety profile, granted not exactly with this vaccine, but with, a very similar vaccine. So I think that it’s clear that vaccination is going to prevent serious illness and death across all age groups. It is a vaccine preventable disease. And so I, for that reason, favor universal recommendation.
Now having said that, I, because I think it’s important for people to have access to the vaccine, if they want it.
Having said that, I also want to say that there’s not equal risk across all ages and populations. And it’s clear that there are certain people, like old people like me, people with underlying medical conditions, that are much higher risk of dying. And so I think that the messaging needs to sort of clarify that and make clear that there is this differential risk, and that a lot of people with underlying medical conditions and who are older are dying, and they really need to get a booster.
…
Barbara Mahon, CDC [03:38:07]
I just wanted to say that, very mindful of the groups that are at substantially higher risk and are planning targeted communications to try to have vigorous and compelling outreach to those groups, that can be done regardless of whether a recommendation is targeted or not.
So under a universal recommendation, we will still have targeted communications for older adults, immunocompromised persons, and others at higher risk.
…
Pablo Sanchez, ACIP [03:55:16]
I just want to be clear that I am not against this vaccine. The data do look great. The limited data that are available does look great, even though it may not be the most, you know, the circulating variants currently, but it has neutralizing activity against the other variants and certainly the ones that are circulating now or expected to be circulating.
I am very much pro vaccination, and certainly high risk groups.
I do— I just want to comment that we have extremely limited data on children and infants and other individuals, and so I think that needs to be made available then to the parents. And I also think that in certain circumstances, we do have to be concerned about potential side effects, especially in the, you know, in young adults and young adult males.
And so I think all of that needs to be weighed. And so that’s why I hesitate to make it just a universal recommendation, even though I do support vaccination with the COVID vaccine.
September 11, 2023
FDA spokesperson on Novavax’s updated COVID vaccine
- Source: email from Cherie Duvall-Jones of the Food and Drug Administration
- Date: received September 11, 2023
Novavax has announced it anticipates the XBB.1.5 composition of its vaccine to be available sometime this fall. Questions about the application’s current status may be directed to the company. As the FDA has done throughout the pandemic, we will make information available as appropriate.
CMS spokesperson on coverage for updated COVID vaccines
- Source: email from a Centers for Medicare and Medicaid Services spokesperson
- Date: received September 5, 2023
The following is provided on background, attributed to the Centers for Medicare & Medicaid Services or a CMS spokesperson:
An FAQ the Departments of HHS, Labor, and Treasury released on October 4, 2021, states in relevant part as follows:
“In a December 12, 2020 meeting, ACIP recommended: “For purposes of ACIP’s role under the Affordable Care Act, ACIP recommends use of COVID-19 vaccines within the scope of the Emergency Use Authorization or Biologics License Application for the particular vaccine.” On the same day, the Director of the CDC adopted this ACIP recommendation. Although ACIP has made additional recommendations regarding COVID-19 vaccines since December 12, 2020, none of those recommendations affect plan and issuer coverage obligations regarding COVID-19 vaccines under the preventive services regulations, and therefore the December 12, 2020 recommendation remains in effect for this purpose. The requirement under section 3203 of the CARES Act for plans and issuers to cover COVID-19 vaccines consistent with this ACIP recommendation became effective 15 business days after the December 12, 2020 adoption by the CDC. Therefore, effective January 5, 2021, plans and issuers must cover, without cost sharing, any COVID-19 vaccine authorized under an EUA or approved under a BLA by the FDA immediately upon the vaccine becoming authorized or approved. This coverage must be provided consistent with the scope of the EUA or BLA for the particular vaccine, including any EUA or BLA amendment, such as to allow for the administration of an additional dose to certain individuals, administration of booster doses, or the expansion of the age demographic for whom the vaccine is authorized or approved.”
The full FAQ can be found here: FAQs about Affordable Care Act Implementation Part 50, Health Insurance Portability and Accountability Act and Coronavirus Aid, Relief, and Economic Security Act Implementation (dol.gov)